The Rising Threat of MPOX Cases: What You Need to Know
Definition and Background of MPOX
MPOX, or Monkeypox, is a viral zoonotic disease caused by the monkeypox virus, typically found in rainforest countries of Central and West Africa. It closely resembles smallpox but is generally less severe. The disease was first identified in laboratory monkeys in 1958, giving it its name. However, the true reservoirs of the virus are believed to be rodents and other small mammals. As cases of MPOX increase globally, understanding its impact has become essential. Symptoms can vary widely and typically include fever, rash, and swollen lymph nodes. The lesions can be painful, appearing in clusters on various parts of the body. Despite being rare, the transmission routes are similar to those of its infamous cousin smallpox, including human-to-human contact through respiratory droplets and direct contact with infected bodily fluids.
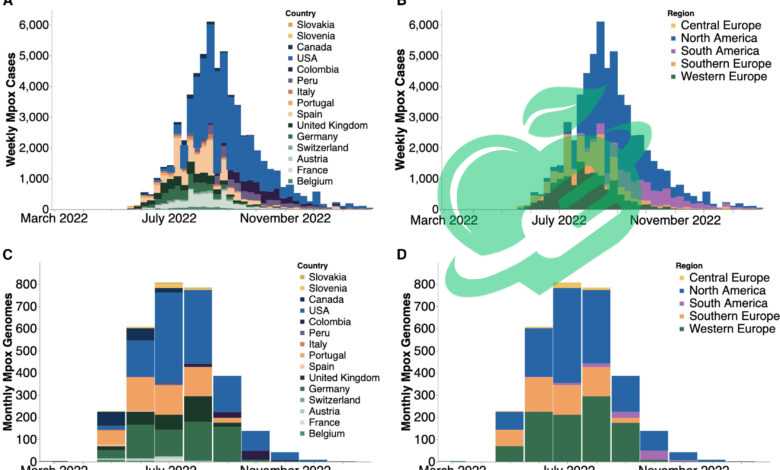
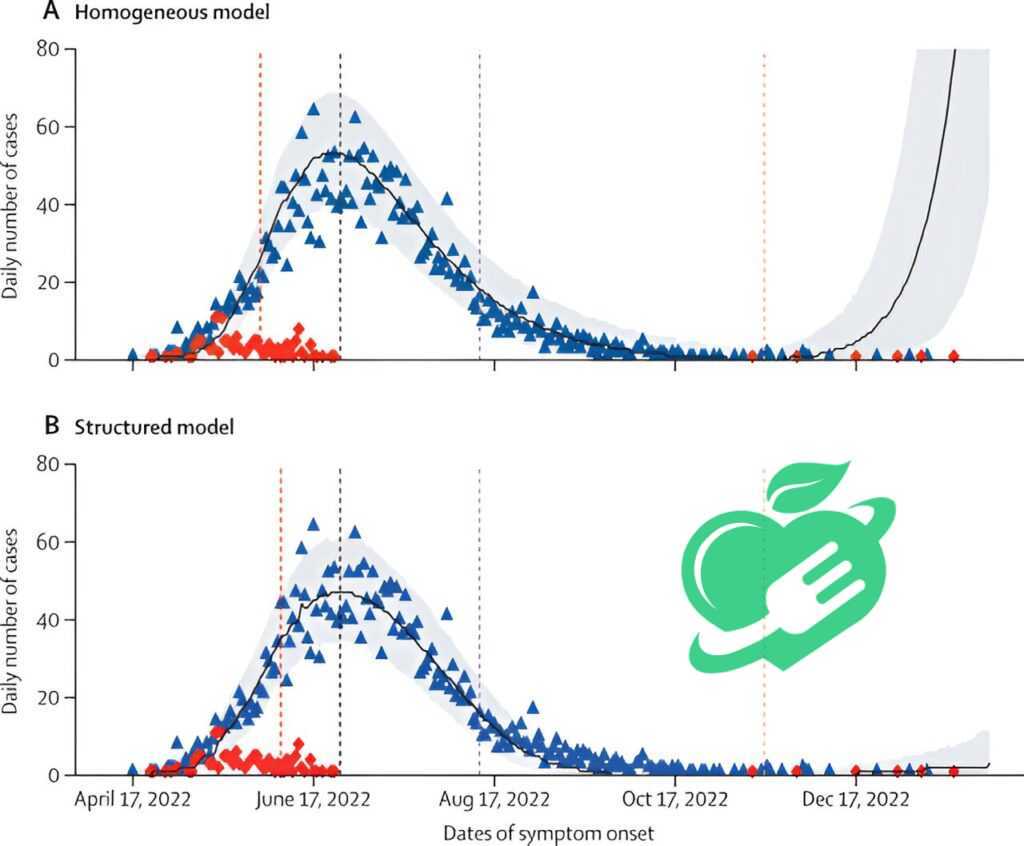
Current Global Situation and Trends
In recent years, there has been a noticeable surge in MPOX cases outside its endemic regions. This rise has drawn considerable attention from public health officials and the scientific community. Key Observations:
- Global Spread: The disease has peaked in non-endemic regions, including North America and Europe, with thousands of reported cases in the past year alone.
- Demographics: The majority of current MPOX cases tend to be in young adults, particularly among men who have sex with men, highlighting the importance of targeted awareness campaigns.
- Increased Awareness: As media coverage grows, communities are becoming more informed about MPOX, resulting in improved detection and diagnosis rates.
Factors Behind the Trend:
- Travel: Global travel has made it easier for diseases to spread.
- Social Interactions: Changes in social behaviors and gatherings have contributed to increased transmission rates.
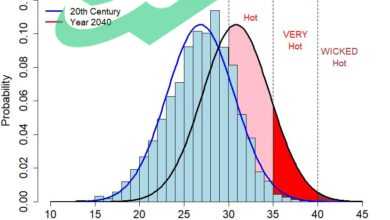
- Ecosystem Changes: Climate change and deforestation may be driving wildlife closer to human populations, increasing the likelihood of zoonotic spillover.
The ongoing rise in MPOX cases underscores the need for urgent epidemiological studies and increased public health interventions. The situation remains fluid, and understanding how to manage this virus effectively is vital for preventing further outbreaks.
Read also: The Ultimate Guide to Boosting Your Health with Lima Beans
Environmental Triggers
The emergence of MPOX cases sheds light on various environmental factors that play a significant role in the disease’s spread. These triggers are often intertwined with human encroachment into wildlife habitats, leading to increased contact between humans and potential animal reservoirs of the virus. Key Environmental Factors:
- Deforestation: As forests are cleared for agriculture or urban development, wildlife habitats are disrupted. This can cause animals that harbor the monkeypox virus to relocate closer to human settlements, increasing the risk of transmission.
- Bushmeat Consumption: In many regions, hunting and consuming wild animals—known as bushmeat—introduces a risk factor. If individuals come into contact with infected animals, such as rodents or primates, they can contract the virus.
- Climate Change: Alterations in climate patterns can disrupt the natural behaviors of wildlife, making them more likely to interact with humans. For instance, warmer temperatures may push certain species into new territories where human populations reside.
Personal experiences from travelers or researchers in endemic regions highlight these environmental links. Many have noted that the proximity to wildlife, combined with local hunting practices, poses a real threat—not just in the field, but reaching urban settings too.
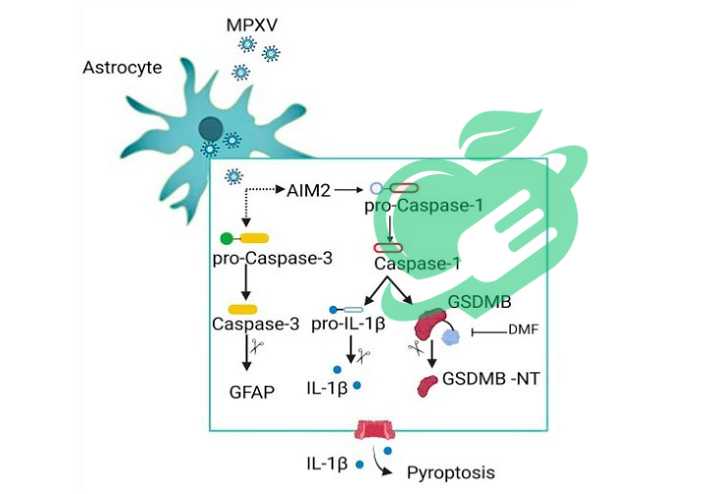
Genetic predisposition to mpox cases
While environmental factors are crucial, genetic predispositions also play a notable role in how individuals respond to MPOX infections. Understanding this aspect helps in identifying vulnerable populations who may be at an elevated risk. Genetic Insights:
- Immune System Variation: Research shows that individuals possess diverse immune system genes, which can affect susceptibility to infectious diseases. Some may lack adequate immune responses to combat viral invasions like MPOX.
- Previous Infections: Those who have been previously exposed to similar viruses, such as smallpox, may carry genetic advantages. Their immune systems might react more robustly compared to individuals without such a background.
Identifying Risk Groups:
- Individuals with compromised immune systems, such as HIV-positive patients, may find their genetic makeup increases their vulnerability to severe outcomes.
- older people, populations can also experience more severe effects due to less resilient immune systems.
Bringing awareness to these genetic factors can aid in public health initiatives, allowing targeted prevention strategies and medical interventions for those at higher risk. Understanding both environmental triggers and genetic predispositions paves the way for a more comprehensive approach to tackling the growing challenge of MPOX.
Read also: What are the fatal health harms of smoking?
Common Presentation
Recognizing the symptoms of MPOX early on is crucial for timely treatment and preventing the spread of the virus. The initial signs can be quite similar to those of other viral infections, which sometimes complicates diagnosis. Typical Symptoms Include:
- Fever and Chills: Patients often report a sudden onset of fever, which can be accompanied by chills and general fatigue.
- Swollen Lymph Nodes: A defining characteristic is lymphadenopathy, which refers to swollen lymph nodes, particularly in the neck and groin areas.
- Rash Evolution: After the onset of fever, a rash typically develops, often starting on the face and then spreading to other parts of the body. This rash can evolve through several stages, from flat spots to raised bumps and ultimately into fluid-filled lesions.
Personal accounts from those recovering from MPOX highlight that the rash can be itchy and painful, significantly impacting daily life. Many describe a challenging journey with constant discomfort, making awareness of these symptoms vital for seeking medical help swiftly.
Diagnostic procedures and tests mpox cases
When it comes to diagnosing MPOX, healthcare professionals rely on a combination of clinical evaluation and laboratory testing, ensuring accuracy and speed in identifying the virus. Diagnostic Steps Include:
- Clinical Assessment: Doctors begin with a thorough medical history and physical exam. They look for classic signs and symptoms of MPOX, particularly the rash and swollen lymph nodes.
- Laboratory Tests: If MPOX is suspected, lab tests become instrumental in confirming the diagnosis. Common testing methods include:
- PCR Test: Polymerase chain reaction (PCR) tests are the gold standard for detecting monkeypox DNA in skin lesions or bodily fluids. This test is extremely sensitive and allows for early detection.
- Serology: Blood tests that look for antibodies specific to monkeypox may also be performed, although they are less commonly used in acute diagnosis.
Confirmation and Reporting: Once a diagnosis is confirmed, public health authorities are notified, facilitating reporting and monitoring of cases. This step is crucial in managing outbreaks and ensuring swift response measures are put into place. Being vigilant about symptoms and understanding the diagnostic process empowers individuals to act promptly. Early detection not only aids in effective treatment but also helps curb the potential spread of MPOX within communities.
Read also: What are the fatal health harms of smoking?
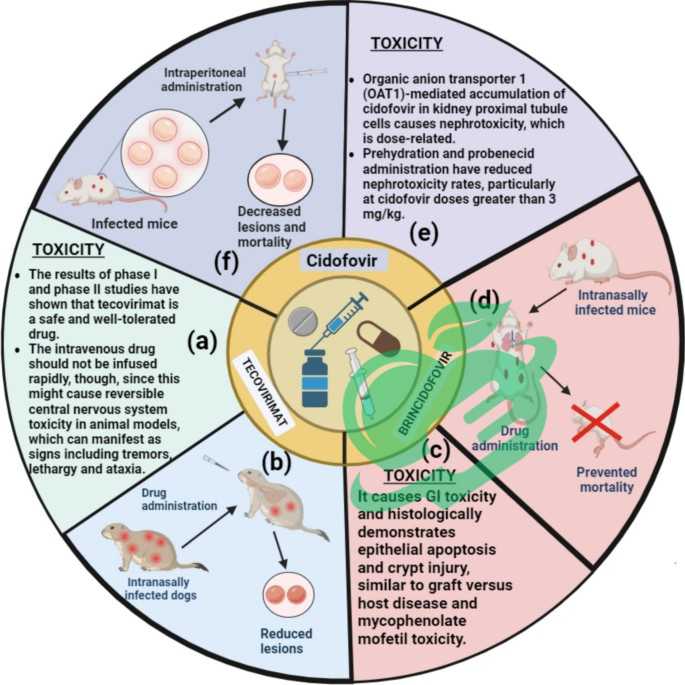
Medications and Therapies – mpox Cases
When it comes to treating MPOX, a thoughtful approach is necessary to alleviate symptoms and promote recovery. Although there is currently no specific antiviral treatment approved for monkeypox, supportive care, and antiviral therapies can significantly help patients manage the illness. Available Options Include:
- Antivirals: Drugs like tecovirimat (TPOXX) have shown promise in treating orthopoxvirus infections, including MPOX. It helps reduce the severity and duration of symptoms.
- Symptomatic Treatment: Depending on the symptoms, treatments may vary. Common approaches include:
- Pain Relief: Over-the-counter medications such as acetaminophen or ibuprofen can help manage fever and alleviate body aches.
- Hydration: Maintaining proper hydration is crucial, especially for patients experiencing fever or skin lesions that may lead to fluid loss.
In personal experiences shared by individuals recovering from MPOX, many emphasize the importance of supportive care—rest, hydration, and monitoring symptoms closely can enhance recovery outcomes. Additionally, some have noted that peer support and community outreach programs play a vital role in emotional well-being during illness.
mpox surgical intervention cases
In more severe cases of MPOX, surgical interventions may sometimes become necessary. These procedures are typically focused on managing complications that arise due to the infection. When Surgical Intervention is Indicated:
- Severe Skin Lesions: In some instances, if skin lesions become infected or extensive with complications, surgical drainage or excision may be considered to prevent further infection.
- Other Complications: If MPOX leads to other serious health problems, such as respiratory distress or secondary infections, surgical options may be pursued to address these issues directly.
Overall, surgical interventions are less common for MPOX but are an important part of a comprehensive treatment plan for severe cases. In conclusion, while existing treatments primarily focus on supportive care and antiviral therapies, staying informed about potential interventions is vital. Education plays a key role, empowering individuals to seek assistance early and effectively manage symptoms, ultimately leading to better recovery experiences. As research continues, hope remains that more targeted treatments for MPOX will become available in the future.
Read also: From Theory to Reality: Exploring the Feasibility of Blood Tests for Anxiety Disorders

Lifestyle changes mpox cases
Preventing MPOX requires a proactive approach, and lifestyle changes play a pivotal role in reducing the risk of transmission. By understanding how personal habits can impact health, individuals can make informed choices that enhance their safety. Key Lifestyle Modifications Include:
- Hygiene Practices: Washing hands frequently with soap and water or using hand sanitizer can help prevent the spread of many viruses, including MPOX. Good hygiene is particularly crucial after contact with potentially contaminated surfaces or animals.
- Avoiding Contact: Reducing contact with wild animals or even pets that may have been exposed to wild animals can significantly lower transmission risk. This is particularly important in regions where monkeypox is endemic.
- Social Distancing: During outbreaks, maintaining physical distance from others, especially from infected individuals, can minimize spread.
- Education and Awareness: Staying informed about the symptoms and transmission routes of MPOX can empower individuals to act quickly if they suspect exposure.
By incorporating these lifestyle changes, individuals contribute to a healthier community. Many who have adopted these practices share personal stories of how increasing awareness in their circles not only benefited them but also helped others feel more secure during a concerning health crisis.
Read also: Uncovering the Truth: The Reality of Leprosy in Florida
How can monkeypox be prevented?
Following certain preventative steps can aid in minimizing or avoiding monkeypox infections. These steps include:
- Getting the smallpox vaccine is advised, as reports suggest that it lowers the likelihood of contracting monkeypox. This vaccine can be particularly beneficial for those who are at high risk of the disease.
- Stay away from animals that could potentially carry the monkeypox virus, including those that are ill or dead animals encountered in regions where the virus is common.
- Steer clear of any materials that have been in contact with animals or humans infected with the virus, including items like bedding and clothing.
- Separate patients infected with monkeypox from individuals who may be at risk of becoming infected.
- Maintain proper hygiene after interacting with infected individuals or animals by thoroughly washing your hands with soap and water or using alcohol-based hand sanitizers.
- Wear personal protective gear when providing care to individuals infected with the disease.
- Practice safe sex, by using condoms.ion in public health.
Economic Burden – mpox Cases
The surge in MPOX cases significantly impacts public health, manifesting in various economic burdens on societies already grappling with healthcare costs. The financial implications of managing an outbreak extend beyond hospital bills, affecting both individuals and healthcare systems. Key Economic Factors Include:
- Healthcare Costs: The expenses incurred by health facilities to diagnose, treat, and manage MPOX cases can strain resources. This includes:
- Increased Hospitalization: Patients with severe symptoms may require prolonged hospital stays, leading to rising healthcare costs.
- Public Health Resources: Health departments need funding to conduct contact tracing and community education, diverting resources from other essential services.
- Impact on Employment: During outbreaks, employees may face loss of income due to illness or enforced isolation.
- Example: A recent report highlighted that a community affected by MPOX saw a significant number of workers unable to attend their jobs, leading local businesses to suffer financially.
- Economic Slowdown: Prolonged health emergencies can deter tourism and affect local economies, especially in areas reliant on visitor traffic. Fear of infection might lead to reduced travel, impacting sectors such as hospitality and retail.
Ultimately, the economic strain from MPOX is a stark reminder of the interconnectedness of health and economics, influencing everyone in society.
Social Implications
Beyond the economic hardships, MPOX also poses significant social implications that ripple through communities. The psychological and relational effects can be profound. Social Challenges Include:
- Stigmatization: There is often a stigma associated with infectious diseases, particularly when transmission is linked to certain demographics.
- Personal Account: Some individuals have shared their experiences of being ostracized from community spaces or social circles after being diagnosed, which can lead to feelings of isolation and depression.
- Public Anxiety: The uncertainty surrounding an outbreak can result in increased anxiety levels within communities. Families may become overly cautious, leading to decreased social interactions or collective activities.
- Community Cohesion: In times of crisis, communities may rally together to support those affected, fostering strength and solidarity. However, fear can also lead to division, highlighting disparities in trust toward healthcare systems.
Many communities are utilizing this experience as an opportunity to strengthen public health messaging and foster community resilience, emphasizing the importance of support networks. In conclusion, the impact of MPOX on public health extends far beyond the individual, creating an economic burden and social challenges that require collective action and thoughtful responses from all sectors of society. Through understanding and addressing these challenges, communities can emerge stronger and better prepared for future health crises.
Read also: Uncovering the Truth: Does Ginger Really Help with Weight Loss?
Emerging Trends
As the world grapples with the increasing cases of MPOX, several emerging trends are shaping the future outlook on how we can combat this viral disease. Understanding these trends enables public health officials, researchers, and communities to adapt proactively. Key Emerging Trends Include:
- Focus on Surveillance: Enhanced disease surveillance systems are being implemented globally. This involves:
- Data Sharing: Countries are collaborating to share data on monkeypox cases, facilitating quicker response times to outbreaks.
- Technological Advances: Innovative technologies, such as mobile health applications, are helping to track symptoms and provide guidance on when to seek treatment.
- Increased Awareness and Education: More resources are being directed towards educating the public about MPOX. Campaigns are focusing on:
- Community Workshops: These workshops emphasize hygiene practices, awareness of symptoms, and the importance of timely medical intervention.
- Targeted Messaging: Health authorities are tailoring information to reach populations at higher risk, enabling better understanding and prevention strategies.
- Integration of One Health Approach: The interconnectedness of environmental, animal, and human health is being recognized more than ever. This approach encourages:
- Collaboration Among Disciplines: Veterinarians, ecologists, and health professionals are teaming up to monitor zoonotic diseases more effectively.
Ongoing Studies and Innovations
Research and innovation are critical in the fight against MPOX, with multiple studies underway focusing on various aspects of the disease. These efforts aim to improve prevention, treatment, and ultimately, the management of outbreaks. Examples of Ongoing Research Include:
- Vaccine Development: Researchers are working on developing vaccines specifically for MPOX. Studies are exploring newer formulations and delivery methods to enhance efficacy.
- Therapeutic Agents: Investigations into antiviral drugs continue, with several trials examining the effectiveness of existing medications against MPOX. This includes:
- Combination Therapies: Researchers are looking at how existing antiviral agents can be used in conjunction with newer drugs to enhance their effectiveness.
- Longitudinal Studies: Long-term research is being conducted to understand the effects of MPOX on various populations, including potential impacts on mental health in those who have recovered.
Over-the-counter treatments
Several over-the-counter remedies are available to help manage the symptoms of monkeypox, including pain, mouth sores, and itching. These treatments consist of the following:
Paracetamol helps alleviate headaches, pain, and fever related to monkeypox.
Non-steroidal anti-inflammatory drugs (NSAIDs) like naproxen and ibuprofen can help alleviate the redness, swelling, and pain linked to monkeypox. It is essential to consider the correct and appropriate dosages based on the patient’s condition.
Antihistamines like cetirizine and loratadine can help alleviate the itching caused by monkeypox; however, it is advised not to drive or operate heavy machinery while taking these medications, as they may lead to tiredness and sleepiness. Additionally, topical treatments such as lidocaine gel, calamine lotion, and ointments or creams that contain corticosteroids or antihistamines can be used to soothe pain and itching on the skin.
Eye drops, including those with antihistamines, decongestants, and artificial tears, can be used to alleviate symptoms of blepharitis or conjunctivitis in certain instances of monkeypox.
Ointments and mouth rinses that include benzocaine, hydrogen peroxide, or chlorhexidine are used to alleviate mouth ulcers and the pain they cause.
Antidiarrheal medications like loperamide and bismuth subsalicylate can be utilized for diarrhea resulting from monkeypox, while electrolyte-rich rehydration solutions are recommended if the patient is experiencing dehydration due to intense diarrhea.
Prescription treatments
You should receive the smallpox vaccine if you’ve come into contact with someone infected with monkeypox, ideally within 4 days of exposure to the virus source, but no later than 2 weeks. This vaccination may also be supplemented with one or more antiviral medications.
Tecoform
It is typically recommended for treating smallpox in individuals who weigh at least 13 kilograms, and the Centers for Disease Control and Prevention are currently researching and testing its use for monkeypox.
Tecovirimat is the preferred choice when over-the-counter treatments fail to manage the symptoms related to monkeypox.
The research related to Tecoformat consists of two distinct pathways:
The STOMP Trial investigates the effectiveness of Tecoformat in treating monkeypox, focusing on comparing the reactions of severe cases to those of moderate cases when Tecoformat is administered orally.
The Expanded Access to New Drugs (EA-IND Protocol) is aimed at treating severe cases of monkeypox under specific conditions, allowing the administration of Tecoformat either orally or intravenously.
Cidofovir
This antiviral, resembling a nucleotide, is typically used to treat cytomegalovirus (CMV) or herpes virus infections. While cidofovir’s effectiveness against the monkeypox virus remains unverified, it might be administered alongside Tecoformat through intravenous injections for severe cases of the disease.
Brincidofovir
This is the inactive version of cidofovir, which can be used for various age groups, including newborns and women who are pregnant or breastfeeding. However, it is important to avoid using both cidofovir and brincidofovir simultaneously.
Brincidofovir is indicated for monkeypox infections under specific circumstances, such as when the individual experiences severe symptoms or has a high risk of the disease progressing, along with one or more of the following factors:
- The infected individual is unable to use Tecoformat or has not been able to do so.
- The infected individual experiences intense side effects while using Tecoformat, or they may respond positively to it initially but then experience a relapse later on.
- The infected individual experiences significant immunodeficiency, similar to those with uncontrolled HIV infection, which necessitates the simultaneous use of brincidofovir and tecovirimat.
- Involvement in the research regarding the application of Tecoformat for the treatment of monkeypox, specifically in the open treatment group C (Arm C).
Trifluridine
Trifluridine is recommended for certain individuals with eye infections caused by monkeypox, and its use is monitored by an ophthalmologist.
Home remedies
Incorporate a series of steps that aid in alleviating and recovering from monkeypox, along with the administration of treatments recommended by the physician, which include the following:
Frequently wash your hands or thoroughly sanitize them after coming into contact with exposed ulcers or blisters.
Gargle with water and salt.
- Make an effort to remain at home as much as you can, or keep to a designated room if others in the family are also present in the house.
- Put on a mask and cover the sores if you are near others or in their company during the disease’s incubation period.
- Refrain from scraping, shaving, or cutting blisters or skin ulcers to prevent them from spreading to other areas of the body or from healing slowly.
Advice
You can consult a doctor to learn about areas where monkeypox is common so you can steer clear of them or take precautions to prevent infection.
Additionally, a doctor can help you recognize the symptoms related to the disease, which can indicate when it is necessary to begin the appropriate treatment based on your specific condition.



One Comment