Unraveling the Mystery: Common Triggers of Painful Urination
Definition of Painful Urination
Painful urination, medically known as dysuria, refers to the discomfort, burning sensation, or pain experienced while urinating. It’s a symptom that’s often more than just an annoyance — it can indicate underlying medical conditions that may require attention. Imagine experiencing a sharp sting every time you go to the bathroom; such an experience is not only uncomfortable but can also disrupt daily life. Painful urination can occur in varying degrees, ranging from mild discomfort to severe pain, and it may manifest differently in each individual. Understanding the context behind painful urination is essential. It usually occurs in conjunction with increased urgency and frequency of urination, which can further complicate one’s experience, leading to anxiety or fear about needing to use the restroom in public or in inconvenient situations.
Common Symptoms Associated with Painful Urination
While painful urination is often the primary symptom, it typically doesn’t exist in isolation. Those suffering from this condition may experience a range of accompanying symptoms. Here are some common ones to watch for:
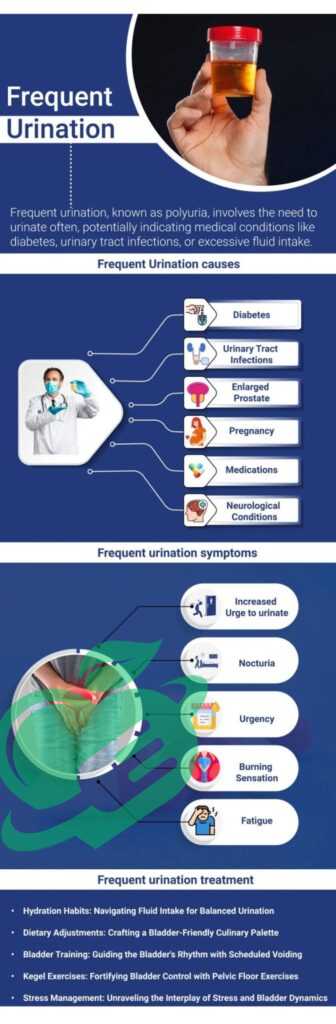
- Increased Frequency: A person may feel the need to urinate more often than usual, even if only small amounts come out each time.
- Urgency to Urinate: There may be an overwhelming feeling that one needs to go to the bathroom immediately.
- Cloudy or Unusual Urine: The urine may appear cloudy or have an unusual odor, which can indicate infection or other issues.
- Blood in Urine: Hematuria (blood in urine) can be alarming and often necessitates immediate medical evaluation.
- Pelvic or Lower Abdominal Pain: Discomfort in the bladder or lower abdomen can accompany painful urination, signaling irritation or infection.
- Fever or chills: These symptoms could suggest a more serious infection, requiring prompt medical attention.
It’s important to note that while some individuals may dismiss these symptoms, especially if they are mild, they should not be taken lightly. Painful urination often indicates underlying health issues that could escalate if left unaddressed. In our fast-paced world, it’s easy to overlook personal health. However, greater awareness of your body’s signals is vital. Take note of any symptoms that accompany painful urination; this vigilance could be key in ensuring timely treatment and management of potential health conditions. Transitioning towards understanding the causes and risk factors of painful urination is an essential next step in addressing this common yet troubling symptom.
Read also: Headaches from MS? Discover the Best Remedies.

Causes of Painful Urination
After grasping the discomfort of painful urination and its associated symptoms, it’s essential to delve into its causes. Understanding the root of the problem can empower individuals to seek appropriate treatment. Here are some common culprits behind this distressing symptom.
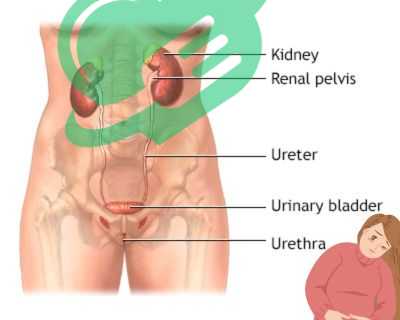
Urinary Tract Infections (UTIs)
One of the most prevalent causes of painful urination is a urinary tract infection (UTI). UTIs occur when bacteria invade any part of the urinary system, including the bladder, urethra, or kidneys. Symptoms of a UTI often include:
- A strong, persistent urge to urinate
- A burning sensation while urinating
- Dark, cloudy, or even strong-smelling urine
- Pelvic discomfort
UTIs are particularly common among women due to their shorter urethras. Personal anecdotes reveal that many women often experience them multiple times in their lives, prompting a search for preventive strategies. Staying hydrated and promptly urinating after intimacy can be beneficial measures.
Sexually Transmitted Infections (STIs)
Sexually transmitted infections (STIs) are another significant cause of painful urination. Conditions like chlamydia and gonorrhea can inflame the urethra, resulting in discomfort during urination. Besides painful urination, STIs may also present symptoms such as:
- Unusual discharge from the genitals
- Swelling or pain in the genitals
- Abdominal pain
Many individuals find it uncomfortable to discuss STIs, but awareness and honesty about sexual health are crucial. Regular screenings and open conversations with partners can promote better sexual health.
Kidney Stones
Kidney stones form when minerals and salts crystallize in the kidneys. As stones progress through the urinary tract, they can cause severe pain, particularly when they irritate the lining of the urinary passages. Signs of kidney stones may include:
- Intense pain in the lower back or side
- Nausea or vomiting
- Blood in the urine
Experiencing kidney stones can be a painfully memorable experience for many. Maintaining a balanced diet and proper hydration can help prevent their formation.
Interstitial Cystitis
Interstitial cystitis (IC), or painful bladder syndrome, is a chronic condition characterized by bladder pressure and pelvic pain. Unlike other causes, IC doesn’t stem from a bacterial infection but rather from inflammation of the bladder walls. Common indicators of IC include:
- Chronic pelvic pain
- Urgency and frequency of urination
- Pain during intercourse
Living with IC is often a long-term struggle for many individuals, with flare-ups and remission cycles. Adopting stress-reduction techniques and dietary changes may provide some relief. Transitions toward understanding the risk factors associated with painful urination will further clarify why some individuals may be more prone to these conditions than others.
Read also: Why Does the Top of My Head Hurt? Find Out Now
Risk Factors for Painful Urination
Now that we have explored the common causes of painful urination, it’s equally essential to look at the risk factors that might make certain individuals more susceptible to this condition. Understanding these factors can lead to better prevention and early intervention strategies.
Gender Differences
Gender plays a significant role in the likelihood of experiencing painful urination. Women are generally more prone to urinary tract infections (UTIs) due to physiological differences. The female urethra is shorter, which makes it easier for bacteria to travel to the bladder. Several insights into gender differences include:
- Anatomy: Women’s anatomy provides a shorter route for bacteria to invade the urinary tract.
- Hormonal Fluctuations: Changes in hormone levels, particularly around menstruation, can affect the urinary tract’s resilience.
- Menstruation and Pregnancy: Women may experience increased susceptibility during these periods due to anatomical changes or hormonal shifts.
Conversely, men can face their unique challenges. Conditions like prostatitis (inflammation of the prostate) can lead to painful urination, highlighting the importance of awareness across genders.
Read also: 11 reasons that may cause infertility
Age-Related Risk Factors
Age also plays a critical role in the risk of painful urination. As people age, urinary health can change significantly. Consider the following age-related factors:
- Children: Young children may suffer from urinary tract infections due to improper toilet habits or anatomical issues.
- Adolescents: This age group may experience STIs more frequently, contributing to painful urination.
- Adults: Middle-aged individuals will need to be cautious of symptoms that may arise due to lifestyle factors, such as dehydration.
- Seniors: People older than 70 often face a decline in bladder control and an increased prevalence of conditions like IC or benign prostate enlargement in men, leading to more urinary complications.
Behavioral Risk Factors
Certain lifestyle choices can heighten the risk of painful urination. Being aware of these can encourage proactive health decisions. Key behavioral risk factors include:
- Poor Hydration: Inadequate water intake can lead to concentrated urine, irritating the bladder.
- Hygiene Practices: Neglecting proper hygiene or safe sex practices can increase the risk of infections and STIs.
- Urinary Habits: Holding in urine for prolonged periods can lead to irritation and increase the probability of infections.
- Diet: A High intake of irritants such as caffeine, alcohol, and spicy foods may aggravate bladder sensitivity.
Encouraging a balanced diet, adequate hydration, and a focus on hygiene could shift these behaviors toward promoting better urinary health. As we continue to build our understanding of painful urination, exploring the diagnosis and treatment options will be the next essential step to empower individuals facing this discomforting symptom.
Read also: Top 10 High Phosphorus Foods to Boost Your Health.

Diagnosis and Treatment of Painful Urination
Having explored the various risk factors associated with painful urination, the next vital step is understanding how this condition is diagnosed and treated. Recognizing symptoms and seeking appropriate medical evaluation is crucial for the effective management of painful urination.
Medical Evaluation and Tests
If an individual is experiencing painful urination, a visit to a healthcare provider is a wise first step. During this evaluation, the doctor will typically conduct a thorough medical history and physical examination. They may ask questions such as:
- How long have you been experiencing painful urination?
- Are there any other symptoms accompanying the pain?
- Do you have a history of urinary tract infections or STIs?
Following this initial assessment, tests may be performed to identify the root cause. Common diagnostic tests include:
- Urinalysis: A urine sample tests for the presence of bacteria, blood, or other abnormalities.
- Urine Culture: If bacteria are found, this test identifies the specific type causing the infection, which helps determine the best treatment.
- Imaging Tests: Techniques such as ultrasounds or CT scans may be used to spot kidney stones or other structural issues.
- Cystoscopy: In some cases, a thin tube with a camera may be inserted into the bladder to visualize any problems directly.
Throughout this process, maintaining clear communication with healthcare providers is essential. Sharing all details about symptoms can lead to more accurate diagnoses.
Treatment Options for Painful Urination
The treatment for painful urination truly depends on the underlying cause. Here are some common options:
- Antibiotics: For bacterial infections like UTIs or STIs, antibiotics are the typical course of action. Following through with the whole course is important, even if symptoms start to improve.
- Pain Relief Medications: Over-the-counter pain relievers such as ibuprofen may provide temporary relief.
- Bladder Training: For conditions like interstitial cystitis, bladder training and physical therapy may be recommended to reduce urgency and frequency.
- Dietary Changes: Individuals are often encouraged to avoid irritants like caffeine, spicy foods, and alcohol.
Personal experiences often reveal that sticking with a treatment plan can significantly improve symptoms and enhance quality of life.
Read also: Vaginitis Unveiled: Symptoms, Treatments, and Prevention
Preventive Measures and Lifestyle Changes
Prevention is key when it comes to painful urination. Implementing a few lifestyle changes can drastically reduce the risk. Consider these preventive measures:
- Stay Hydrated: Drinking plenty of water can help flush out toxins and bacteria.
- Practice Safe Sex: Using protection can significantly lower the risk of STIs.
- Maintain Good Hygiene: Adopting proper hygiene habits, such as wiping front to back after using the bathroom, can reduce the risk of infections.
- Regular Check-ups: Routine visits to healthcare providers can help catch any potential issues early on.
Implementing these changes not only decreases the development of painful urination but also fosters overall urinary health. Transitioning from this understanding of diagnosis and treatment into the next conversations around when to seek medical help for painful urination is crucial for emphasizing the importance of timely action.
Read also: Empower Your Health: Recognizing and Addressing 8 Triggers of Vaginal Pain.

When to Seek Medical Help for Painful Urination
Understanding the signs of painful urination and when to seek medical help is crucial for managing this condition effectively. While mild symptoms may sometimes resolve on their own, certain warning signs should never be overlooked. Recognizing these red flags can ultimately make a significant difference in one’s health.
Red Flags and Warning Signs
Being vigilant about the symptoms of painful urination can help individuals identify when professional help is necessary. If any of the following signs accompany urinary pain, it’s time to reach out to a healthcare provider:
- Persistent Symptoms: If painful urination lasts longer than a day or two without improvement, don’t wait to seek help.
- Blood in Urine: Finding blood in urine, known as hematuria, is a serious sign and warrants immediate attention.
- Severe Abdominal or Back Pain: Experiencing sharp or severe pain in the lower abdomen or back, especially if persistent, can indicate kidney stones or other serious conditions.
- High Fever or Chills: These symptoms can signify a severe infection that may require urgent treatment.
- Nausea or Vomiting: When these accompany painful urination or back pain, they may indicate a kidney issue or severe UTI.
- Difficulty Starting or Stopping Urination: If there’s an unexpected interruption in urination, it could suggest blockage or other complications.
By recognizing these warning signs, individuals can take proactive steps to address their health needs. A friend’s experience, where delayed medical attention for painful urination led to a severe kidney infection, serves as a sobering reminder of the importance of timely action.
Importance of Timely Medical Intervention
Timely medical intervention cannot be overstated when it comes to managing painful urination. Acting quickly can prevent minor issues from escalating into more complex, serious conditions. Here’s why seeking medical help promptly is vital:
- Prevent Complications: Untreated infections can lead to complications such as chronic kidney disease or sepsis, putting one’s health at significant risk.
- Receive Appropriate Treatment: Early diagnosis allows for specific treatments tailored to the underlying cause, whether that’s an infection, stone, or another issue.
- Improve Quality of Life: Rapid relief from symptoms can lead to a better quality of life, allowing individuals to return to normal activities without discomfort.
- Educate on Prevention: Engaging with healthcare professionals early on provides the opportunity to learn preventive measures tailored to their circumstances.
Ultimately, being proactive about urinary health pays dividends. Recognizing the importance of timely intervention encourages individuals to take their symptoms seriously and prioritize their well-being. As we wrap our understanding of painful urination, it’s essential to recognize that knowledge and vigilance are key components in managing one’s health effectively. Awareness of symptoms, risk factors, and when to seek help sets individuals up for success in their journey toward urinary wellness.
Read also: Peeing After Sex: The Key to Better Intimacy Health.
Tips for Managing and Preventing Painful Urination
Now that we’ve explored when to seek medical help for painful urination, it’s time to focus on proactive measures. Managing and preventing this discomfort involves a combination of hydration, diet, personal hygiene, and ongoing care. By making small adjustments in daily habits, individuals can improve their urinary health significantly.
Hydration and Diet Tips
Staying hydrated is a cornerstone in both preventing and managing painful urination. Water plays a crucial role in flushing toxins from the body and diluting urine, which can help prevent irritation. Here are some helpful tips:
- Drink Plenty of Water: Aim for about 8-10 glasses of water daily to keep your urinary system healthy.
- Limit Irritants: Reducing the intake of caffeine, spicy foods, artificial sweeteners, and alcohol can lower the risk of bladder irritation.
- Include Cranberry Products: Some studies suggest that cranberry juice may help reduce the risk of UTIs, though moderation is key due to its acidity.
- Balanced Diet: Incorporating antioxidant-rich fruits and vegetables can support overall health and may benefit urinary function.
A friend of mine found that simply increasing her water intake made a notable difference in her experiences with painful urination. It just goes to show how something as simple as hydration can have a powerful impact!
Read also: The Pelvic Exam: What Every Woman Should Know
Personal Hygiene Practices
Good personal hygiene is another critical facet in managing urinary health. Simple practices can go a long way in preventing infections:
- Wipe Correctly: Always wipe from front to back after using the restroom to reduce the risk of bacteria from the anal region reaching the urethra.
- Urinating after Intercourse: This practice helps to flush out potential bacteria from the urinary tract.
- Cotton Underwear: Opting for breathable fabrics like cotton allows for better airflow, which can help keep the genital area dry and free from bacteria.
- Regularly Change Sanitary Products: For those menstruating, changing tampons or pads frequently prevents bacterial growth.
A colleague once mentioned how making the switch to cotton underwear eliminated her recurrent urinary discomfort. It’s anecdotes like these that highlight the impact of personal care on urinary health.
Follow-up Care and Monitoring
Finally, engaging in follow-up care is vital for ongoing urinary health. Regular check-ups and monitoring can help prevent recurring issues.
- Schedule Routine Doctor Visits: Regular appointments allow for health assessments and early detection of any potential problems.
- Keep a Symptom Diary: Tracking symptoms over time helps identify triggers or patterns that may correlate with painful urination.
- Follow Treatment Guidelines: If prescribed medication or treatment, following the healthcare provider’s recommendations ensures the best chance of resolution.
Frequently Asked Questions
What to drink when it hurts to pee?
If you have a UTI, it’s important to drink ample fluids to keep hydrated, such as water, electrolyte beverages, and cranberry juice. However, it’s best to steer clear of caffeinated beverages like coffee, tea, and energy drinks, as they may exacerbate your UTI symptoms. Additionally, it’s advisable to avoid alcohol during your illness. 1
Why does it burn when I pee but no infection?
What causes a burning sensation in my urethra without an infection? The discomfort at the tip of the urethra can result from irritation caused by sexual activity, masturbation, tight clothing, or certain cleaning products. Additionally, kidney stones and some cancer therapies might lead to a burning feeling during urination. 2
What is the fastest way to cure burning urine?
- Consult a healthcare provider. Generally, UTIs are not considered a serious issue.
- Fill your prescription immediately.
- Use a non-prescription medicine to alleviate the pain and urgency.
- Drink lots of water.
- Go to the bathroom often.
- Drink green tea.
- Avoid alcohol and caffeine. 3
Can a UTI go away on its own?
Occasionally, a urinary tract infection (UTI) may resolve without treatment. However, the majority of individuals will require antibiotics. Some may receive a ‘delayed antibiotic’ prescription, which means they should only take the medication if their symptoms persist after a specified period. 4
How to test for UTI at home?
You can find them at a pharmacy or online without needing a prescription. The home testing kit includes specially coated test strips. You either hold the strips in your urine stream or submerge them in a urine sample. These strips detect nitrites and leukocytes that are commonly found in urinary tract infections (UTIs). 5
Follow us for more updates and breaking news, as we provide you with everything new.
- goodrx ((↩))
- healthline ((↩))
- goodrx ((↩))
- bhf ((↩))
- healthlinkbc ((↩))




I’m extremely impressed with your writing talents as well as with the layout to your weblog. Is this a paid topic or did you modify it yourself? Anyway keep up the excellent high quality writing, it’s rare to see a nice weblog like this one nowadays!