Headaches from MS? Discover the Best Remedies

Understanding Multiple Sclerosis (MS) Headaches
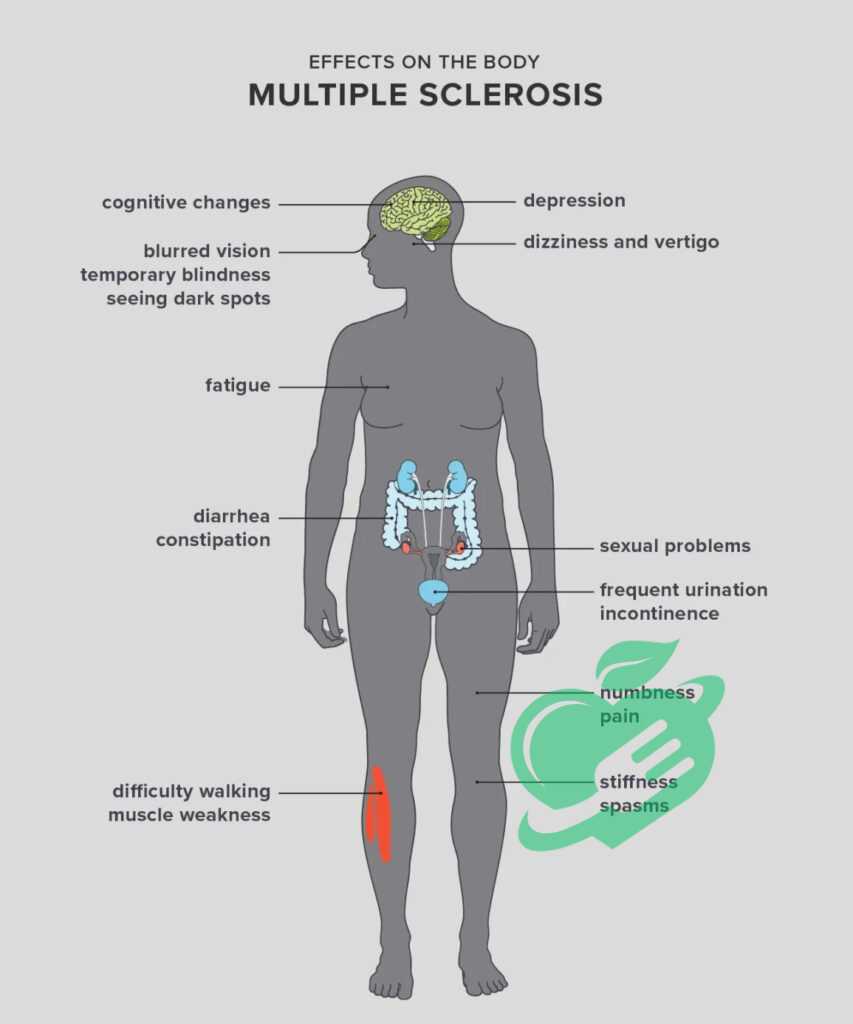
Multiple Sclerosis, commonly referred to as MS, is a progressive neurological disease that affects the central nervous system. It occurs when the immune system mistakenly attacks the protective sheath (myelin) surrounding the nerve fibers, leading to communication issues between the brain and the rest of the body. The exact cause of MS remains unclear, but it is generally considered to involve a combination of genetic and environmental factors. Managing MS can be a complex journey. People diagnosed with the condition might experience a range of symptoms, including fatigue, balance problems, and cognitive difficulties. But one symptom that often catches many off guard is headaches. Individuals with MS may not initially associate their headaches with their diagnosis, which can lead to confusion and frustration. Common Symptoms of MS:
- Numbness or Tingling: Often in the limbs or face.
- Fatigue: Extreme tiredness not relieved by rest.
- Difficulty Walking: Balance and coordination issues.
- Visual Problems: Blurred vision or double vision.
- Cognitive Changes: Issues with memory or concentration.
Understanding MS is vital for recognizing why headaches may occur. MS can take many forms, categorized chiefly into relapsing-remitting MS and progressive MS, each affecting individuals differently. Those with MS need to be aware of the potential for various headaches, as these can significantly impact their quality of life.
Read also: Sinus Headache SOS: Quick Fixes and Long-Term Solutions.
Relationship between MS and Headaches
The connection between MS and headaches is a complex one that has been the subject of numerous studies. It’s interesting to note that while headaches are not considered a primary symptom of MS, many individuals living with the disease report experiencing them. How MS Influences Headaches:
- Neurological Impacts: MS directly affects the nervous system, which can lead to alterations in how pain is perceived. This altered pain sensitivity may result in tension-type headaches and migraines.
- Inflammation: The inflammatory processes inherent in MS can affect the brain’s pain pathways, possibly triggering headaches. When the immune system is activated in MS, it can create inflammatory molecules that can contribute to headache onset.
- Fatigue and Stress: Living with MS can be incredibly taxing both physically and emotionally. Many find that fatigue and the stress of managing a chronic illness can lead to tension headaches, which are prevalent among those with MS.
- Medication Side Effects: Some treatments for MS, such as certain disease-modifying therapies, can have side effects, including headaches. When polysymptomatic, managing these headaches becomes vital for overall well-being. 1.
Statistics to Consider:
- A significant percentage of people with MS report experiencing migraines or tension-type headaches.
- One study indicated that nearly 50% of individuals with MS experience headaches, compared to the general population.
Personal Reflection
Consider Jane, a 34-year-old diagnosed with relapsing-remitting MS. She often found herself overwhelmed by the fatigue stemming from her condition. In her case, the stress compounded the headaches she experienced, leading her to explore both medical and lifestyle solutions. Jane discovered that making small changes, like practicing yoga and mindfulness, helped alleviate her headache frequency and severity. Understanding the relationship between MS and headaches is crucial for effective management. By recognizing that headaches can interplay with a person’s MS experience, individuals like Jane can seek tailored solutions that address not only their neurological health but also their overall well-being. The path towards effectively managing MS headaches involves looking closely at their triggers and learning to cope with the challenges the condition presents. In the following sections, we’ll delve into the various causes of headaches experienced by those living with MS.
Read also: How to Identify and Treat Allergy-Induced Headaches.
Causes of Headaches in Multiple Sclerosis
In understanding the complexities of Multiple Sclerosis (MS) headaches, it becomes essential to explore the underlying causes. These headaches can arise from several factors related to the neurological and inflammatory nature of the disease, as well as the side effects of medications. Let’s delve into these causes, shedding light on how each contributes to the experience of headaches among those living with MS.
Neurological Factors
The neurological aspects of MS play a significant role in the development of headaches. Given that MS is a disease of the central nervous system, any disruption to normal nerve function can trigger pain. Key Neurological Contributors:
- Demyelination: The damage to the myelin sheath surrounding the nerves can lead to erratic communication within the nervous system. This dysfunction may cause the brain to misinterpret signals, resulting in headache sensations.
- Central Sensitization: Individuals with MS may develop a heightened sensitivity to pain. This means everyday stimuli that wouldn’t typically induce discomfort can become painful, leading to headaches.
- Nerve Root Involvement: As MS progresses, lesions can form on the spinal cord, affecting the nerve roots. This can trigger referred pain, including headaches, due to the interconnectedness of the body’s nerve systems. 2.
A Personal Example: Take the story of David, a 28-year-old MS patient who often experiences relentless tension headaches. After consulting with his neurologist, he learned that the lesions formed on his brain were contributing to his sensitivity to pain. Understanding this connection allowed David to approach his headaches with targeted therapies that addressed nerve function.
Read also: Understanding Meningitis and Its Link to Headaches
Inflammatory Processes
Another significant culprit in triggering headaches among those with MS is the inflammatory processes that accompany the disease. When the immune system mistakenly attacks the myelin, it creates an inflammatory response that doesn’t just affect the nerves but can also lead to various symptoms, including headaches. Inflammatory Mechanisms to Note:
- Cytokine Release: In MS, pro-inflammatory cytokines are released that increase the permeability of blood vessels in the brain. This can lead to a condition known as neurogenic inflammation, where pain pathways in the central nervous system become activated, causing headaches.
- Increased Intracranial Pressure: Inflammation can lead to swelling and increased pressure within the skull, which can cause headaches. People often describe this type of pain as a “pressure” feeling rather than a typical headache.
- Chronic Inflammation: As MS progresses, ongoing inflammation can lead to chronic pain conditions that may manifest as frequent headaches. 3.
Real-World Insight: Sophia, a 40-year-old woman with MS, often noted that her headaches became worse during periods of disease flare-up. Medication to manage her inflammation helped mitigate not only her MS symptoms but also lessened the severity and frequency of her headaches, showcasing the connection between the two.
Medication Side Effects
Finally, the treatment regimen for MS can also contribute to headache occurrences. While many medications are necessary for managing symptoms and slowing the disease’s progression, some can have uncomfortable side effects, including headaches. Common Medication Side Effects:
- Disease-Modifying Therapies (DMTs): Certain DMTs can cause headaches as part of their side effect profile. This includes injection-site reactions or systemic responses that can induce pain.
- Corticosteroids: Medications like corticosteroids, often used during MS exacerbations, can cause headache symptoms in some patients, particularly during dosage adjustments.
- OOver-the-counter(OTC) Medications: Additionally, some individuals may use NSAIDs or other pain relief medications too frequently, leading to rebound headaches.
Example from Experiences: Consider Mark, who was prescribed a new DMT that significantly improved his MS symptoms but also triggered periodic headaches. After discussing this with his healthcare provider, they adjusted the medication plan and incorporated preventive strategies, which helped Mark gain better control over his headaches. Navigating the causes of headaches related to MS involves understanding the intricate interplay between neurological factors, inflammation, and medication. Recognizing these causes will pave the way to effective management strategies, which will be the focus of the upcoming sections.
Read also: Headaches on Repeat: A Guide to Your Daily Struggle.
Types of Headaches Associated with MS
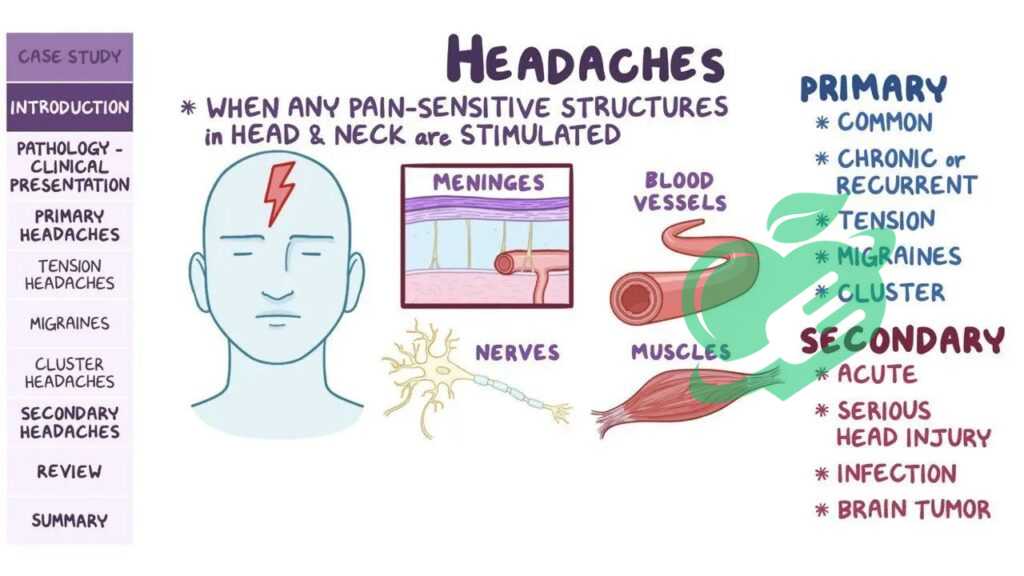
Understanding the types of headaches that can occur in individuals with Multiple Sclerosis (MS) provides valuable insights into managing this often-overlooked symptom. As explored previously, the causes of headaches in MS can be multifaceted; however, the manifestation of these headaches can also differ significantly among individuals. Below, we will discuss three primary types of headaches associated with MS: tension headaches, migraines, and cluster headaches.
Tension Headaches
Tension headaches are the most commonly reported type of headache among individuals with MS. These headaches are typically characterized by a dull, aching pain accompanied by a sensation of tightness or pressure across the forehead, temples, or back of the head and neck. Key Features of Tension Headaches:
- Intensity: Generally mild to moderate.
- Duration: Can last from 30 minutes to several days.
- Associated Symptoms: Often not accompanied by nausea or vomiting, which distinguishes them from migraines.
- Triggers: Stress, fatigue, poor posture, and muscle tension can contribute to the onset of these headaches. 4.
Personal Anecdote: Take Emily, a 45-year-old woman living with MS, who began experiencing frequent tension headaches during stressful workdays. After realizing that long hours at her computer were exacerbating her symptoms, she introduced regular breaks and stretching into her routine. This simple shift significantly reduced her tension headaches and improved her overall comfort during work.
Migraines
Migraines are another type of headache that MS patients may experience. While not everyone with MS suffers from migraines, a good number do report them. Migraines can be debilitating and are often characterized by intense, throbbing pain, usually on one side of the head. Characteristics of Migraines:
- Intensity: Moderate to severe, often interfering with daily activities.
- Duration: Typically lasts from four hours to three days if untreated.
- Associated Symptoms May include sensitivity to light, sound, or smell; nausea; and vomiting.
- Aura: Some individuals experience auras, which are visual or sensory disturbances that precede the headache, including flashes of light or tingling in the limbs.
Expert Insight: Research suggests that MS patients may experience a higher prevalence of migraines compared to the general population. Example: Consider Thomas, a young father with MS who described his migraine attacks as “explosions” of pain. He found that keeping a headache diary helped identify triggers such as dietary choices and changes in weather, leading him to implement strategies like dietary adjustments and preventive medications. By understanding his migraine patterns, Thomas was able to take proactive steps to reduce their frequency.
Cluster Headaches
Cluster headaches, although less common, are another type of headache that can occur in individuals with MS. These headaches are characterized by intense pain on one side of the head and often occur in cyclical patterns (clusters). Unique Aspects of Cluster Headaches:
- Intensity: Severe, often described as a piercing or burning sensation.
- Duration: Episodes can last from 15 minutes to three hours, often occurring multiple times a day.
- Associated Symptoms: Nasal congestion, watery eyes, and restlessness during episodes.
- Timing: They often follow a predictable pattern, occurring at the same time each day.
Real-World Perspective: Jessica, a 38-year-old woman with MS, shared her experience with cluster headaches. During a recent episode, she was unable to sit still and felt compelled to pace. Finding relief was challenging, but with the guidance of her healthcare provider, she discovered triptans, a class of medication effective in treating cluster headaches. The experience of headaches in individuals with MS is diverse and can significantly impact daily life. By recognizing the different types of headaches associated with MS, patients can better communicate their symptoms to healthcare providers, leading to tailored treatment and management strategies. In the following sections, we will explore managing and relieving headaches in individuals with MS, offering valuable tools for those affected.

Managing and Relieving MS-Related Headaches
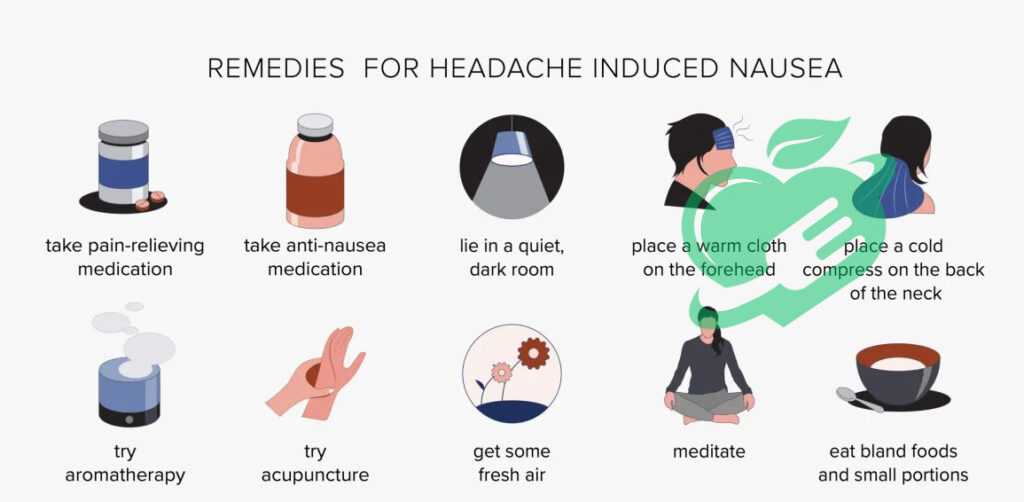
Having explored the various types of headaches associated with Multiple Sclerosis (MS), it’s crucial to discuss strategies for managing and relieving these discomforts. Headaches can profoundly impact daily life, but with the right approach, effective relief is possible. This section will cover medication options, lifestyle changes, and alternative therapies, providing a comprehensive toolkit for individuals living with MS.
Medication Options
When it comes to managing MS-related headaches, medication can play a significant role. Healthcare providers often recommend various options, allowing patients to find what works best for their unique situations. Common Medication Categories:
- Over-the-Counter Analgesics: Non-prescription medications like ibuprofen or acetaminophen can serve as first-line treatments for milder headaches, including tension headaches.
- Prescription Medications: For more severe headaches or migraines, doctors may prescribe medications such as:
- Triptans: These are often effective for migraines and work by constricting blood vessels and minimizing inflammation.
- Preventive Medications: Beta-blockers and anticonvulsants may help patients with chronic migraines manage their symptoms over the long term.
- Muscle Relaxants: If tension headaches arise from muscle tightness, muscle relaxants may provide relief. 5.
Personal Testimony: David, a 32-year-old MS patient, found success with a combination of preventive medication and over-the-counter pain relievers. Initially, he struggled with debilitating migraines, but after consulting his neurologist, he started a regimen of daily low-dose amitriptyline, which significantly reduced his headache frequency. Individuals need to workk closely with their healthcare providers to tailor medication plans that fit their specific needs and symptoms.
Lifestyle Changes
In addition to medication, lifestyle adjustments can also play a critical role in managing headaches associated with MS. By making small, meaningful changes, individuals can significantly improve their quality of life and reduce headache frequency. Effective Lifestyle Modifications:
- Stress Management: Incorporating calming practices such as yoga, meditation, or deep-breathing exercises can help alleviate tension and reduce headaches.
- Regular Sleep Patterns: Establishing a consistent sleep schedule can combat fatigue and decrease the likelihood of headaches. Aim for 7-9 hours of quality sleep each night.
- Adequate Hydration: Dehydration can trigger headaches, making it essential to drink enough water throughout the day.
- Physical Activity: Regular exercise helps reduce stress levels and tension. Even moderate activities like walking or gentle stretching can be beneficial.
Anecdote of Improvement: Sophia, who struggled with tension headaches, decided to incorporate regular yoga sessions into her weekly routine. Not only did she find relief from headaches, but she also noticed improved flexibility and a better overall mood. This holistic approach helped Sophia embrace her MS experience with a more positive outlook.
Read also: Brain Freeze Buster: Remedies for Instant Relief
Alternative Therapies
For those seeking relief beyond traditional medication and lifestyle changes, alternative therapies may offer additional avenues for managing MS-related headaches. Many individuals have found success incorporating these practices into their overall treatment plans. Popular Alternative Therapies:
- Acupuncture: This traditional Chinese medicine technique has been shown to reduce headache frequency and intensity for some individuals by improving blood flow and promoting relaxation.
- Chiropractic Care: Regular visits to a chiropractor can help relieve tension in the neck and shoulders that often leads to headaches, particularly tension headaches.
- Herbal Supplements: Some people find relief with herbs like butterbur and feverfew, known for their anti-inflammatory properties. Consulting with a healthcare provider before starting any new supplements is crucial.
Testimonial from Experience: Mark, who frequently battled migraines, began acupuncture sessions after hearing positive reports from friends. To his delight, he found that not only did his headache frequency decrease, but the treatment also provided a sense of relaxation and overall well-being. As this section illustrates, managing and relieving MS-related headaches is a multidimensional process. By combining medication with lifestyle modifications and exploring alternative therapies, individuals can create a tailored approach to their headache management. In the upcoming sections, we will delve into practical tips for preventing MS headaches, further empowering individuals on this journey.
Read also: Why Does the Top of My Head Hurt? Find Out Now
Tips for Preventing MS Headaches
Building on the previous discussion about managing and relieving MS-related headaches, prevention is crucial. Individuals living with Multiple Sclerosis (MS) can adopt specific strategies to help reduce the likelihood of headaches and improve their overall quality of life. This section explores stress management techniques, maintaining a healthy diet, and ensuring regular exercise and sleep patterns.
Stress Management Techniques
Stress is a well-known trigger for headaches, particularly for those with MS. Therefore, effective stress management techniques can significantly reduce headache frequency and severity. Practical Stress Management Strategies:
- Mindfulness and Meditation: Practicing mindfulness or meditation for just a few minutes daily can promote relaxation and reduce anxiety. Consider guided apps, such as Headspace or Calm, which offer structured sessions aimed at stress reduction.
- Breathing Exercises: Deep breathing exercises can help lower stress levels immediately. Try the 4-7-8 technique: inhale for four counts, hold for seven, and exhale slowly for eight counts.
- Journaling: Some individuals find journaling helpful for processing feelings and managing stress. Setting aside time each day to jot down thoughts or reflect on positive experiences can be beneficial.
- Art and Music Therapy: Engaging in creative activities, whether through painting, playing an instrument, or listening to soothing music, can divert focus from stressors and promote relaxation.
Personal Perspective: Emily, a 39-year-old living with MS, discovered the power of guided meditation surprisingly. When she began incorporating short meditation sessions into her mornings, she noticed a significant decrease in her overall stress levels and a corresponding reduction in tension headaches. These techniques can be simple yet profoundly impactful when integrated into daily life. 5.
Read also: Simple Solutions for Headache Behind Eyes.
Maintaining a Healthy Diet
Diet can play an essential role in headache prevention for those with MS. A balanced and nutritious diet helps maintain energy levels and supports overall well-being. Key Dietary Considerations:
- Stay Hydrated: Dehydration is a common headache trigger. Aim to drink at least eight glasses of water daily, and consider herbal teas or fruits with high water content, such as cucumbers and oranges, for added hydration.
- Incorporate Anti-inflammatory Foods: Foods high in omega-3 fatty acids (such as salmon, walnuts, and flaxseeds) and antioxidants (such as berries, leafy greens, and nuts) can help reduce inflammation and may lower headache frequency.
- Avoid Trigger Foods: Some individuals find that specific foods can trigger headaches. Common culprits include aged cheeses, processed meats, caffeine, and alcohol. Keeping a food diary can help identify any potential triggers in your diet.
- Regular Meal Timing: Skipping meals can provoke headaches. Eating small, balanced meals throughout the day can stabilize blood sugar levels and help manage fatigue.
Anecdote from Experience: Sophia shifted her eating habits after recognizing patterns between her meals and headache occurrences. By focusing on whole foods and eliminating processed snacks, she noticed not just a reduction in headaches but also an increase in her overall energy levels.
Regular Exercise and Sleep Patterns
Regular physical activity and consistent sleep patterns are integral to managing overall health and may significantly impact headache prevention. Effective Strategies:
- Exercise Routine: Aim for at least 150 minutes of moderate exercise each week. This can include activities such as walking, cycling, swimming, or gentle yoga. Exercise releases endorphins, which act as natural pain relievers.
- Listen to Your Body: While regular exercise is important, it’s equally crucial to listen to your body and not overdo it. On days when fatigue sets in, opt for lighter activities like stretching or a leisurely walk.
- Establish a Sleep Schedule: Consistency is key when it comes to sleep. Aim for 7-9 hours each night, going to bed and waking up at the same time daily. Creating a relaxing bedtime routine can signal to your body that it’s time to wind down.
- Create a Comfortable Sleep Environment: Ensure your bedroom is conducive to sleep—dark, cool, and quiet—and avoid screens at least an hour before bedtime to promote better rest.
Personal Testimony: Mark, a 36-year-old MS patient, struggled with sleep disturbances and noticed that when he prioritized a consistent sleep schedule, his headaches significantly reduced. He also added gentle morning stretches to his routine, which helped him feel rejuvenated and less prone to tension headaches. In conclusion, implementing these preventive strategies can empower individuals with MS to take control of their headache management. By focusing on stress management, a healthy diet, and regular exercise and sleep patterns, they can foster a healthier lifestyle that may lead to a reduction in headache occurrences. As we move forward, it’s essential to continue exploring the various facets of living well with MS.
- practicalneurology ((↩))
- ncbi ((↩))
- nationalmssociety ((↩))
- msplus ((↩))
- medicalnewstoday ((↩))((↩))




Thanks for sharing. I read many of your blog posts, cool, your blog is very good.