Brain Damage Posturing: What You Must Know

Understanding Brain Damage Posturing
Brain damage posturing is a crucial concept within neurology and emergency medicine. It refers to a range of abnormal body positions that can occur when there is significant injury to the brain. These postures are typically indicative of severe neurological impairment, often resulting from conditions like traumatic brain injury, stroke, or severe oxygen deprivation. Let’s break down what this means. Imagine a 30-year-old individual who was in a serious car accident. After the accident, rather than responding normally, the person may exhibit specific postures that indicate how their brain is processing trauma. These postures serve as non-verbal cues to healthcare providers, helping to gauge the severity of the injury and guide subsequent treatment decisions. These abnormal posturing responses can manifest in a few distinct forms, which we will explore further, but they generally signal an inadequate reaction from the brain to external stimuli.
Causes of Brain Damage Posturing
Understanding what leads to brain damage posturing is essential for both prevention and treatment. The causes can be varied and complex, embedding within themselves numerous health issues. Here are some of the most common causes:
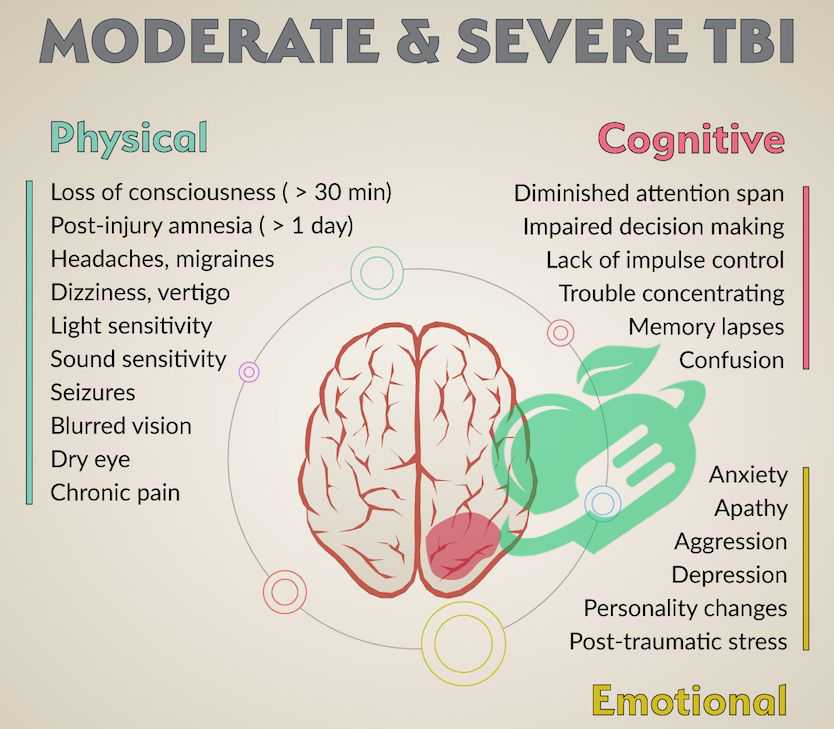
- Traumatic Brain Injury (TBI): This is one of the leading causes of brain damage posturing. TBIs can result from falls, car accidents, sports injuries, or violence.
- Stroke: A stroke occurs when blood flow to the brain is disrupted, either due to a blockage (ischemic stroke) or a burst blood vessel (hemorrhagic stroke). This lack of oxygen can lead to posturing.
- Lack of Oxygen: Conditions such as drowning or suffocation can lead to brain damage. When the brain doesn’t receive adequate oxygen, it can manifest as abnormal posturing.
- Severe Infections: Conditions like bacterial meningitis can severely impact brain function and lead to posturing.
- Metabolic Disorders: Disorders that disrupt the chemical balance in the body, such as liver failure or kidney failure, can also cause brain injury, contributing to abnormal posturing. 1.
Moreover, those suffering from significant brain trauma may experience various forms of posturing as their bodies react to the injury. It’s fascinating to observe how the brain’s health directly affects physical body responses; thus, each abnormal posture serves as a critical indicator of the underlying brain condition. Recognizing these causes not only aids medical professionals in diagnosis but could potentially help in crafting preventative strategies. Understanding the full scope of how brain damage posturing operates can also offer insights into the complex interplay between injury and the body’s response, reinforcing why timely intervention is so vital. By keeping a keen eye on the circumstances leading to such posturing, both individuals and healthcare providers can work towards reducing the risks of severe brain damage.

Types of Brain Damage Posturing
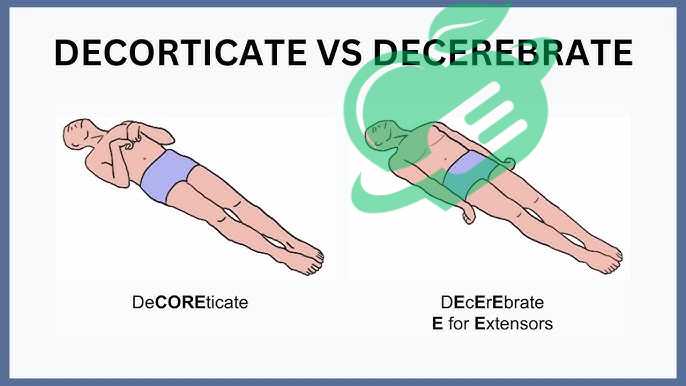
After gaining an understanding of the causes of brain damage posturing, it’s essential to delve into the specific types that medical professionals recognize. One of the most significant forms is decorticate posturing. This type occurs when there is damage to the brain, particularly to the cerebral hemispheres or the pathways that communicate with the spinal cord. So, what does decorticate posturing look like? A patient demonstrating this condition typically has their arms flexed, hands clenched into fists, and legs extended. This stance can be alarming to witness, as it often indicates a severe underlying brain injury. Imagine visiting a friend in the hospital following a traumatic accident and seeing them in this stiff position. It’s a gut-wrenching sight, as you know it reflects their battle with brain health. Here are some key characteristics of decorticate posturing:
- Arm Position: Arms are flexed toward the chest.
- Leg Position: Legs are extended straight out.
- Symptoms: Patients may also have altered levels of consciousness, confusion, or unpredictable movements.
Understanding this posture is vital, as it signals the need for immediate medical assessment and intervention. It’s crucial to note that while decorticate posturing is a serious symptom, it often carries a better prognosis than its counterpart, decerebrate posturing. 2.
Decerebrate Posturing
On the other side of the spectrum is decerebrate posturing, often considered more severe and potentially indicative of deeper brain dysfunction. This posture is characterized by the arms being extended straight out, with wrists and fingers also extended. The legs are stiff and extended as well, making the body appear rigid. Witnessing someone in this position can be utterly devastating. A family may find themselves observing such posturing in their loved one after a stroke or full-scale brain trauma, which can feel like a rollercoaster of emotions—hope mixed with despair. Key characteristics of decerebrate posturing include:
- Arm Position: Arms are extended straight out at the sides.
- Leg Position: Legs are rigid and may be straight out.
- Symptoms: Patients may exhibit more severe levels of consciousness impairment, and this type often signifies significant brain injury, particularly in the brainstem region.
Here’s a comparative breakdown of the two types of posturing for clarity:
| Type | Arm Position | Leg Position | Indication of Severity |
|---|---|---|---|
| Decorticate Posturing | Flexed toward the chest | Extended straight | Generally better prognosis |
| Decerebrate Posturing | Extended straight out | Rigid and extended | More severe brain dysfunction |
Recognizing these types of posturing helps healthcare providers determine the extent of brain injury and offers families some insight into what might be happening with their loved ones. Understanding the nuances between decorticate and decerebrate posturing enables better communication with healthcare professionals, enhancing the entire patient care experience.
Read also: Brain Freeze Buster: Remedies for Instant Relief.
Signs and Symptoms
Now that we’ve explored the types of brain damage posturing, it’s crucial to recognize the signs and symptoms that may indicate a serious brain injury. Understanding these indicators can be lifesaving, both for the individual experiencing them and for those around them. When observing someone who may have sustained a brain injury, several key signs should alert you to seek immediate medical assistance:
- Abnormal Body Posturing: This includes decorticate and decerebrate posturing, as previously discussed. Witnessing these postures can often be an immediate red flag.
- Altered Consciousness: If a person is confused, lethargic, or unresponsive, it may signify serious brain impairment.
- Severe Headache: A sudden, severe headache, often described as a “thunderclap” headache, can indicate issues like a hemorrhagic stroke or ruptured aneurysm.
- Nausea and Vomiting: Unexplained nausea or repetitive vomiting, especially after head trauma, requires careful attention.
- Loss of Coordination: Clumsiness, trouble balancing, or difficulty walking can be symptomatic of brain injury.
- Vision Changes: Blurred or double vision, or even sudden loss of vision, can all indicate brain problems. 3.
Imagine you’re at a family gathering, and you notice your uncle struggling to keep his balance and slurring his words. These signs can be worrying and should not be dismissed as mere fatigue.
Diagnosis and Assessment
The process of diagnosing brain damage, posturing, and the underlying causes begins with a thorough assessment by medical professionals. Quick and accurate evaluation is key to ensuring appropriate treatment. Here’s how the diagnostic process typically unfolds:
- Initial Evaluation: Healthcare providers will begin by asking questions about the incident, medical history, and any observed symptoms. This can help gauge the severity of the injury.
- Neurological Examination: A detailed neurological exam will assess various functions, including reflexes, coordination, and consciousness levels. Tools like the Glasgow Coma Scale (GCS) help quantify the level of consciousness and dictate further action.
- Imaging Tests: Typically, imaging tests such as a CT scan or MRI are conducted to visualize the brain’s structure and identify any bleeding, swelling, or other structural issues.
- Additional Tests: Depending on the situation, blood tests or EEGs might also be employed to rule out infections or assess brain activity.
- Continuous Monitoring: Often, patients are monitored continuously in a hospital setting for any changes in condition, which is critical for timely intervention.
This rigorous diagnosis process can be complex and time-consuming, but it’s essential for ensuring that the best treatment options are pursued. Having a reliable healthcare team that can recognize these signs and assess them effectively can make all the difference in recovery. Understanding the signs and symptoms of brain damage posturing, as well as the rigorous assessment process, can empower friends and family members to act quickly in emergencies, ultimately leading to better outcomes for those affected.
Read also: Best Tips for Crushing It on the Running Track
Treatment and Management
Following the diagnosis of brain damage posturing, medical interventions become critical in preventing further injury and promoting recovery. The immediate response will largely depend on the underlying cause of the posturing and the patient’s overall condition. In an emergency scenario, your loved one may face interventions such as:
- Medications: Depending on the diagnosis, medications may be used to reduce swelling in the brain, manage symptoms, or prevent seizures. For example, corticosteroids can help minimize inflammation around the injury.
- Surgery: In some cases, surgical intervention may be necessary, especially if there’s bleeding or significant pressure on the brain. Imagine a situation where a family member has sustained a brain hemorrhage: a neurosurgeon may need to perform a craniotomy to relieve pressure and prevent further damage.
- Supportive Care: This includes monitoring neurological status, ensuring proper oxygenation, and managing vital signs. Sometimes, a patient may need to be intubated to assist with breathing, especially if they are unresponsive.
- Intravenous (IV) Fluids: IV fluids may be administered to keep the person hydrated and maintain blood pressure, providing crucial support as doctors stabilize their condition.
Prompt medical intervention can significantly impact recovery and outcomes, making timely action essential. For families, understanding what to expect from initial medical treatments can help during a challenging time.
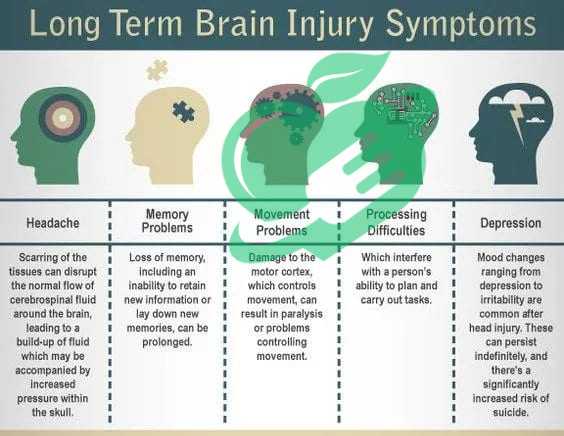
Rehabilitation and Long-Term Care
Once the patient is stabilized, the focus shifts to rehabilitation and long-term care, an equally vital phase in their recovery journey. Rehabilitation aims not only to address physical impairments but also cognitive and emotional challenges that may arise from brain injury. Consider the roadmap of rehabilitation:
- Physical Therapy (PT): This helps patients regain strength, coordination, and mobility. Imagine someone struggling to take their first steps after an injury—PT guides them every step of the way to rebuild muscle memory and balance.
- Occupational Therapy (OT): OT focuses on helping patients regain daily living skills, such as dressing, grooming, and even cooking. For example, someone may need retraining in basic skills following brain damage affecting motor functions.
- Speech and Language Therapy: For individuals who experience difficulties with speech or swallowing, speech therapy plays a crucial role in restoring communication and safe eating.
- Psychological Support: Emotions can run high post-injury. Counselors or psychologists assist patients and families in coping with the emotional aftermath of brain injuries, including anxiety and depression.
- Ongoing Monitoring and Follow-up Care: Regular follow-ups with neurologists and rehabilitation specialists ensure that progress is tracked and adjustments to treatment plans are made as needed. 4.
Read also: How to get rid of chronic foot pain?
Prognosis and Recovery of brain damage posturing
As we reflect on treatment and management, it’s essential to consider the prognosis for individuals exhibiting brain damage posturing. Prognosis varies significantly from case to case, influenced by various factors that can dictate the path of recovery. Understanding these elements can provide insight into what families might expect as they navigate this challenging journey. Several key factors can affect the prognosis of individuals with brain damage:
- Severity of the Injury: The extent and location of the brain injury play a crucial role. For instance, a mild concussion may have a much better prognosis than a severe traumatic brain injury.
- Response to Initial Treatment: Quick and effective medical intervention can improve outcomes dramatically. For example, a patient who receives immediate surgery for a hematoma may recover better than one who delays treatment.
- Age and Overall Health: Younger individuals typically recover better than older adults due to greater neuroplasticity, which allows the brain to reorganize and adapt. Additionally, pre-existing health conditions, such as diabetes or heart disease, can complicate recovery.
- Presence of Complications: Complications such as infections, seizures, or additional brain injuries can hinder recovery and worsen the prognosis.
- Support System: A strong network of family and friends can provide emotional and practical support that may positively influence recovery. For example, a family member actively involved in rehabilitation can significantly encourage motivation and improvement.
These factors combined can create vastly different outcomes for individuals impacted by brain damage posturing. Families must keep these elements in mind as they advocate for the best possible care and rehabilitation for their loved ones.
Rehabilitation results for brain damage posturing
Rehabilitation is often a multidimensional process focused on restoring independence and quality of life. The outcome of rehabilitation varies widely based on individual circumstances, yet several common experiences can help paint a picture for families. Key considerations for rehabilitation outcomes include:
- Individualized Treatment Plans: Rehabilitation services are tailored to address specific impairments. This personal approach often leads to better results. For example, a customized physical therapy program targeting a patient’s unique challenges can significantly enhance mobility outcomes.
- Time Frame for Recovery: Recovery from brain injuries can take weeks, months, or even years, depending on the severity of the damage. Families should remain patient and stay engaged in the rehabilitation process to foster motivation and resilience.
- Cognitive and Emotional Recovery: It’s not just about physical mobility. Many individuals may experience cognitive challenges that require specialized support from neuropsychologists or occupational therapists, enabling them to regain skills needed for daily living.
- Quality of Life Assessments: Rehabilitation outcomes are often measured not just by physical capabilities, but also by improvements in emotional well-being and social integration, which can provide a more comprehensive view of recovery.
- Long-term Adaptations: Some individuals may need ongoing support even after rehabilitation ends. Connecting with community resources, support groups, or in-home care can facilitate continued growth and adaptation.
Recovery from brain damage is a dynamic and ongoing process. Engaging in rehabilitation actively creates opportunities for improvement and adaptation, paving the road for a fulfilling life after injury. Families who remain informed and involved can help their loved ones achieve the best possible outcomes and navigate the complex world of recovery together.
Read also: Choosing the Best Diet for Enhancing Brain Health

Prevention and Safety Measures
As we continue exploring the complexities surrounding brain damage posturing, it’s crucial to shift our focus toward prevention. Taking proactive measures to avoid brain injuries can save countless individuals and families from the upheaval associated with such conditions. Preventing brain injuries begins with awareness and education. Here are some fundamental strategies to help reduce the risk of brain injuries:
- Wear a Helmet: Whether biking, skateboarding, or participating in contact sports, wearing a properly fitted helmet can significantly reduce the risk of traumatic brain injuries. For instance, when my younger brother started cycling, our family made it a rule to always wear helmets. This simple habit instilled a culture of safety that set the tone for our outdoor activities.
- Use Seatbelts: Always buckle up, both as a driver and passenger. Vehicle crashes are a leading cause of brain injuries, and using seatbelts can drastically reduce the risk of serious harm.
- Prevent Falls: Falls are a common source of brain injuries, particularly among older adults and children. Installing handrails, non-slip mats, and safety gates in homes can mitigate these risks. When my grandmother moved in with us, we made it a priority to remove trip hazards and ensure her safety.
- Educate on Sports Safety: Coaches, parents, and athletes should actively learn about concussions and implement safety protocols. Practicing safe techniques in sports can protect players from serious head impacts.
- Safe Environments at Work and Home: Implement safety measures that create hazard-free environments. For example, using protective gear for employees in high-risk jobs can prevent injuries. 5.
These preventative measures form the foundation for a safer life, emphasizing that being proactive is often the first line of defense against brain injuries.
Read also: Unveiling the Mysteries of Yoga: A Comprehensive Beginner’s Handbook.
Safety Guidelines for Avoiding Brain Damage posturing
After understanding prevention, it’s essential to incorporate safety guidelines that individuals can adopt in various scenarios. Here are effective tips to enhance safety and minimize the risk of brain damage:
- Regular Health Check-ups: Keeping up with regular medical check-ups allows for the identification of underlying health issues. High blood pressure and heart disease can increase brain injury risks, so managing these conditions is vital.
- Mindfulness and Attention: Be aware of your surroundings, especially in high-risk scenarios. Simple actions, like not texting while walking or maintaining focus while driving, can prevent accidents.
- Childproofing the Home: For families with young children, childproofing homes can prevent falls and accidents. Secure sharp corners, use corner guards, and anchor heavy furniture to prevent tipping.
- Emergency Preparedness: Teaching children and adults about emergency procedures during accidents plays a critical role in ensuring quick and effective responses. Knowing how to react can minimize injury severity.
- Educating the Community: Engaging in community safety initiatives can promote awareness. Local workshops that focus on safety in various environments—homes, schools, and workplaces—can create a culture of prevention.
By integrating these safety guidelines into daily routines, families and communities can work together to mitigate the risk of brain injuries. The more informed and proactive individuals are about safety measures, the better equipped they are to protect themselves and others from potential tragedies. As communities come together to foster a culture of safety and awareness, we pave the way toward a future with fewer brain injuries, significantly reducing the challenging journeys that follow such events.
The importance of early recognition and intervention for brain damage posturing
As we wrap up our exploration of brain damage posturing, one key takeaway remains clear: early recognition and intervention are paramount in addressing brain injuries effectively. The sooner signs of brain damage are recognized, the better the chances for recovery and rehabilitation become. Consider a scenario where a sports player receives a blow to the head during a game. If coaches, teammates, and family recognize the potential signs of a concussion, like confusion or unusual behavior, immediate action can be taken to seek medical care. I recall attending a school football game where a player was quickly removed from the field after showing signs of disorientation. Fortunately, prompt medical attention resulted in a positive outcome with no long-term consequences. Here are several reasons why early recognition is so critical:
- Immediate Care: Rapid treatment can prevent further injury. Delays can exacerbate the situation, leading to complications that might have been avoided with timely intervention.
- Improved Recovery Rates: The quicker medical interventions occur, the more favorable the prognosis. With robust rehabilitation plans commencing earlier, patients often see better outcomes.
- Family and Community Support: When families are better informed and actively engaged in recognizing symptoms, they can create supportive environments that substantially influence recovery.
Early detection acts as a catalyst for both medical and emotional support, ensuring that individuals facing brain damage are ushered toward a path of healing and resilience.
Read also: Preventing and Managing Brain Bleed: What You Need to Know.
Future Research and Development
Looking ahead, the landscape of brain injury treatment and management is constantly evolving, with research paving new pathways for hope and improvement. Despite the challenges posed by brain damage, advancements in medical science and technology continue to offer promising avenues for the future. Potential areas for growth and research include:
- Advanced Imaging Techniques: Innovations in neuroimaging, like functional MRI, can help doctors better understand patterns of brain injury and develop targeted treatments tailored to the unique needs of each patient.
- Gene Therapy: Research into genetic therapies may eventually unlock new ways to repair or regenerate neural tissue, offering hope for patients with severe brain injuries.
- Telehealth and Remote Rehabilitation: The rise of telehealth services, accelerated by recent global events, allows patients greater access to specialized care regardless of geographical barriers. This advancement could enhance rehabilitative support and patient monitoring.
- Community Awareness Programs: More comprehensive education regarding brain injury prevention and recognition can be developed and promoted within schools, sports organizations, and public health initiatives.
Frequently asked questions
What part of the brain causes decerebrate posturing?
Decerebrate rigidity occurs as a result of damage to the midbrain. This condition leads to heightened extensor positioning in the limbs, including the neck, and increased reflexes in the lower limbs, and it is associated with a poor outlook for recovery. Trauma is the leading cause of such midbrain injuries. 6.
What part of the brain controls posturing?
The cerebellum is located at the rear of the brain. It is responsible for coordinating voluntary muscle movements and plays a role in maintaining posture, balance, and stability. 7.
Why do hands curl up after brain injury?
Spasticity is a frequent neurological symptom that arises after a traumatic brain injury. It is marked by an unusual rise in muscle tone, resulting in the hand muscles becoming rigid or tightening simultaneously when the patient attempts to move, stretch, or relax them. 8.
Is decerebrate posturing reversible?
While the occurrence of decerebrate posturing usually suggests irreversible conditions, when it appears in conjunction with hepatic encephalopathy, it should be viewed as a potentially reversible condition that might not result in any lasting harm to the patient. 9.
What is the fencing position for brain injury?
The fencing response refers to an abnormal positioning of the arms that occurs after a concussion. This reaction happens right after the brainstem experiences moderate force, during which the forearms remain either flexed or extended (usually raised) for several seconds following the impact. 10.
Because your health is the most valuable thing you have and the most precious thing we care about, we always recommend that you consult your specialist doctor in everything related to your health and daily life. Everything we provide here is for awareness purposes only and does not replace consulting a doctor. Every person has a unique condition that deserves special care, and we are here by your side, working passionately to provide the information you need. Always follow us, because we write for you with love and sincerity to remain a source that inspires you with hope and supports you on your journey towards a better life.
- medlineplus ((↩))
- en.wikipedia ((↩))
- mountsinai ((↩))
- ncbi ((↩))
- shepherd ((↩))
- ncbi ((↩))
- urmc.rochester ((↩))
- neuliferehab ((↩))
- pmc ((↩))
- Wikipedia ((↩))



