Breaking Down Health Disparities for Better Health Equity

Understanding Health Disparities
Health disparities refer to the profound differences in the quality of health and healthcare experienced by different populations. This frequently includes variations in incidence, prevalence, mortality, and burden of diseases. When one group suffers from worse health outcomes compared to another, it exemplifies the concept of health disparities. To put it simply, if a community has limited access to health services or experiences higher rates of chronic illnesses like diabetes, these variations depict health disparities. For instance, in San Bernardino, health disparities are evident, where certain demographics, especially low-income families, face significant barriers in accessing healthcare resources.
Factors Contributing to Disparities
Several factors contribute to health disparities, and understanding these variables is crucial for developing effective solutions. Here are some significant contributors:
- Socioeconomic Status: Individuals from lower socioeconomic backgrounds often have limited access to healthy food, safe environments, and quality healthcare services.
- Education: A higher level of education is associated with increased awareness of health issues and better healthcare navigation.
- Location: Rural areas often lack healthcare facilities, making it challenging for residents to receive timely care.
- Cultural Beliefs: Cultural factors can influence health-seeking behavior and access to treatment. For example, some communities may prefer traditional medicine over conventional approaches.
- Discrimination: Historical and systemic racism can systematically disadvantage certain groups, leading to poorer health outcomes.
These factors don’t operate in isolation; they intersect, creating compounded barriers for individuals. For instance, a single mother living in poverty might struggle to find childcare while trying to get a medical appointment, illustrating how varying layers of difficulty can entrench health disparities.
Impact of Health Disparities on Communities
The impact of health disparities on communities is immense and multifaceted.
- Worsening Overall Health: When health disparities exist within a community, the overall health of that community is jeopardized. Higher rates of illness lead to increased healthcare costs and reduced workforce productivity.
- Economic Strain: Communities facing health disparities often confront higher rates of absenteeism, increased emergency care, and chronic disease management costs, which can place a heavy financial burden on local healthcare systems and economies.
- Social Cohesion: Disparities can erode trust, leading to weakened social ties. Individuals who perceive systemic barriers may disengage from community initiatives aimed at improving health.
In conclusion, understanding health disparities requires not just defining them but also recognizing the intricate web of factors that contribute to these inequities and the profound effects they have on communities. By addressing these disparities holistically, we can foster a healthier, more equitable society for all.

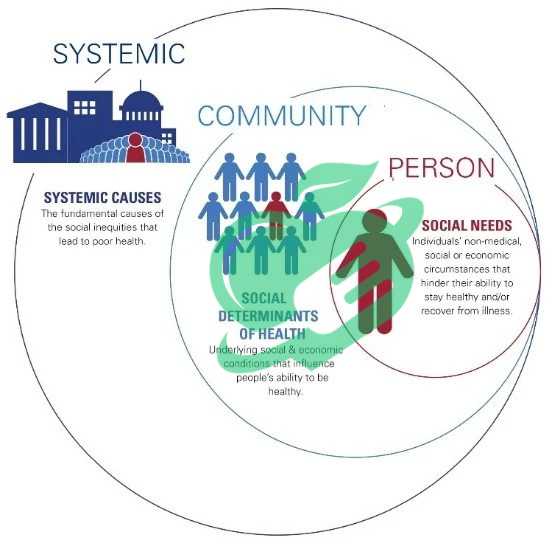
Root Causes of Health Disparities
Understanding the root causes of health disparities is essential for developing targeted interventions. By analyzing these causes, we can see how they intertwine and impact the health of communities differently.
Socioeconomic Factors
Socioeconomic factors play a crucial role in determining health outcomes across different populations. People with lower income levels often face multiple challenges that hinder their ability to maintain good health.
- Income Level: Limited financial resources can restrict access to nutritious food, preventative care, and necessary medications. A person living paycheck to paycheck may choose cheaper fast-food options instead of investing in healthy groceries.
- Education: The education level informs individuals about health practices and resources. For example, a college-educated person is more likely to understand the importance of regular check-ups compared to someone with less educational attainment.
- Employment: Job stability and conditions can also influence health. Those working in hazardous environments or with limited benefits may experience a higher prevalence of work-related injuries or stress-related illnesses.
Reflecting on real communities, many individuals in San Bernardino have shared experiences of struggling to afford basic healthcare or healthy meal options due to their socioeconomic status.
Access to Healthcare
Access to healthcare is a significant determinant of health disparities. Even when individuals recognize the importance of healthcare, various barriers can prevent them from receiving necessary treatment.
- Availability of Services: In many under-resourced areas, clinics may be sparse, making it inconvenient for residents to seek care. Long travel distances can discourage individuals from pursuing routine check-ups or specialist appointments.
- Affordability: High costs associated with healthcare services can act as a deterrent. Many people may forego treatments simply because they cannot afford insurance premiums or out-of-pocket expenses.
- Insurance Coverage: Lack of insurance or underinsurance can be a defining factor in health access. Communities with higher rates of uninsured individuals often see spikes in late diagnoses and advanced stages of diseases.
Individuals in lower-income neighborhoods often cite these issues as significant barriers to seeking timely care.
Environmental Influences
The environment significantly affects health outcomes and can perpetuate disparities. Factors such as living conditions and access to clean air, water, and nutritious food all play a role.
- Pollution: Residents in areas with high pollution levels, often tied to industrial zones, face greater health risks, such as respiratory issues.
- Built Environment: Proximity to parks, grocery stores, and healthcare facilities can foster healthier lifestyles. Communities lacking these resources may contribute to higher obesity rates and mental health issues.
- Housing Quality: Substandard housing often includes issues like lead paint and mold exposure, which can lead to chronic health problems.
Health Disparities: Cultural and Social Determinants
Cultural and social determinants also influence health disparities, as they shape health beliefs and behaviors.
- Cultural Norms: Traditions and beliefs impact how communities perceive health and illness. For instance, some may prioritize holistic practices over traditional medical approaches, which can lead to delayed care.
- Social Support: A strong community network can promote healthy behaviors and encourage individuals to seek medical help when needed. In contrast, communities lacking these ties might experience increased isolation and health challenges.
By addressing these root causes—socioeconomic factors, access to healthcare, environmental influences, and cultural norms—communities can begin to enact effective strategies toward alleviating health disparities. Recognizing these disparities empowers us all to make informed decisions and advocate for equity in health.
Read also: Mental Health in Nursing: Challenges and Solutions
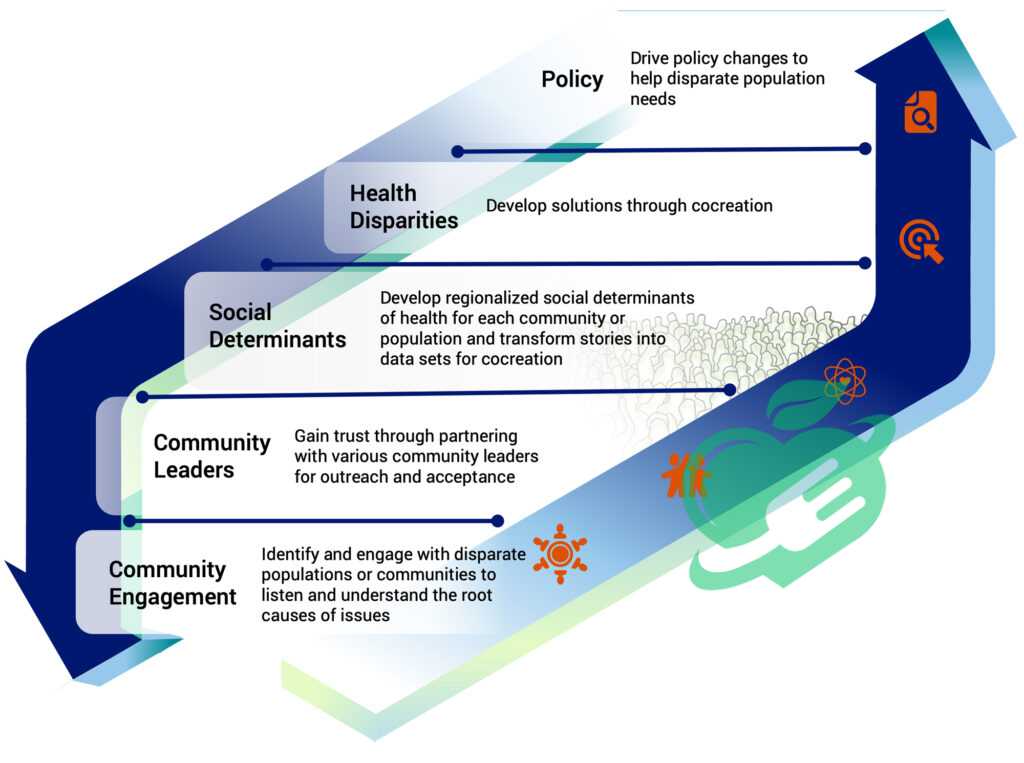
Addressing Health Disparities for Health Equity
Having explored the roots of health disparities, it’s essential to delve into actionable strategies aimed at fostering health equity. Turning the tide in health disparities involves commitment and careful planning across multiple dimensions.
Promoting Health Literacy
Health literacy is the cornerstone of informed health choices. When individuals understand health information, they are more likely to take proactive steps in managing their health. Here’s how to promote health literacy effectively:
- Simplifying Medical Information: Many patients struggle to understand medical jargon. By creating easily digestible materials, such as brochures and videos, healthcare providers can help patients better grasp their health situations.
- Workshops and Training: Community organizations can hold workshops focusing on areas like nutrition, chronic disease management, and navigating healthcare systems. For instance, a local health fair in San Bernardino successfully educated participants on diabetes management, leading many to take charge of their health.
- Utilizing Technology: Mobile apps can serve as interactive tools for managing health, with features designed to increase understanding and motivation.
Conversing with individuals about their experiences highlights how essential health literacy is in making informed choices. Many have shared that a better understanding of their conditions helped them advocate for themselves during medical visits.
Strengthening Healthcare Systems
A robust healthcare system is pivotal in addressing health disparities. Here are some key approaches to strengthening healthcare systems:
- Increasing Workforce Diversity: It’s essential to cultivate a diverse healthcare workforce that reflects the communities they serve. Having practitioners from similar backgrounds can build trust and improve patient experiences.
- Improving Accessibility: Expanding services in underserved areas, such as mobile clinics, can significantly enhance accessibility. For example, mobile health units traveling to rural neighborhoods can provide essential screenings and vaccinations.
- Telehealth Expansion: Investing in telehealth services can break down barriers for those who find physical travel difficult, making it easier for individuals to consult healthcare professionals.
These improvements ensure that care is not only available but also tailored to the unique needs of diverse populations.
Community Outreach and Education
Effective community outreach initiatives are vital for raising awareness about health disparities and promoting healthy behaviors. Some strategies include:
- Building Partnerships: Collaborating with local organizations and schools can bolster outreach efforts. For instance, partnerships with schools can provide students and families with resources and education on preventive health measures.
- Cultural Relevance: Programs should be designed with cultural sensitivity and relevance in mind. Understanding the unique perspectives of various communities can enhance participation and engagement.
- Health Events: Organize health fairs or fun runs to connect the community with health resources while fostering a sense of community. Many families find these events enjoyable and informative.
Policy Interventions
Finally, policy interventions are essential for driving systemic change. Policymakers play a crucial role in establishing regulations that promote health equity:
- Funding and Resource Allocation: Ensuring that healthcare funding is directed toward underserved areas can significantly impact the availability of services.
- Health Equity Legislation: Implementing laws that address systemic barriers, such as anti-discrimination mandates in healthcare, can help create a more equitable system.
- Collecting Data: Policymakers should prioritize collecting data on health disparities to identify trends and assess the effectiveness of existing programs.
By implementing these strategies—promoting health literacy, strengthening healthcare systems, engaging in community outreach, and advocating for policy interventions—we can bridge the gap in health disparities. Together, these efforts create a stronger foundation for lasting health equity, allowing everyone the opportunity for a healthier life.
Read also: Sinus Headache SOS: Quick Fixes and Long-Term Solutions
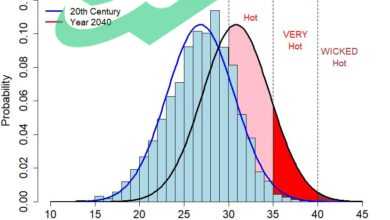
Data-driven Solutions for Health Equity
As we move forward in our efforts to address health disparities, leveraging data-driven solutions becomes essential. Integrating data into our strategies allows for targeted interventions that can significantly improve health outcomes in underserved populations.
Read also: Understanding the Importance of Mental Health First Aid
Utilizing Data to Identify Disparities
The first step in addressing health disparities is identifying which groups are most affected and the specific barriers they face. Utilizing data plays a crucial role in this process.
- Demographic Data: Collecting demographic information helps pinpoint at-risk populations. For example, data revealing higher rates of hypertension within particular racial or socioeconomic groups in San Bernardino can highlight areas of concern.
- Health Surveys: Conducting community health surveys can unveil important insights into residents’ perceptions of healthcare access, quality, and barriers they encounter. These surveys reveal real stories and struggles faced by individuals.
- Geographic Information Systems (GIS): GIS technology enables map-based visualizations that can illuminate areas with high health disparities. For instance, mapping chronic disease rates against access to healthcare facilities enables policymakers to see where urgent interventions are needed.
Having worked with various community organizations, many have shared how this data has opened doors for discussions about the specific needs within their regions, prompting focused advocacy efforts.
Health disparities and implementation of evidence-based interventions
Once disparities are identified, the next step is to implement evidence-based interventions. This approach ensures that funding and resources are directed to effective solutions.
- Pilot Programs: Initiating pilot programs in communities can serve as a testing ground for new health initiatives. For instance, a successful telehealth pilot in a rural area may provide valuable insights into its efficacy before wider implementation.
- Collaboration with Experts: Partnering with researchers and health professionals can help tailor interventions to best fit community needs. Many health initiatives have benefitted from expert collaboration, resulting in higher engagement and success rates.
- Feedback Mechanisms: Establishing feedback loops allows for continuous improvement. Communities should be encouraged to share their experiences to help guide future interventions.
Reflecting on past projects, community leaders often emphasize the importance of evidence-based solutions as they tend to resonate more with the populations they serve, fostering higher participation.
Read also: Dye Disasters? 7 Easy Solutions for Removing Hair Dye from Skin
Monitoring Progress and Outcomes
Lastly, monitoring progress and outcomes is crucial to ensuring interventions are effective and paving the way toward success.
- Data Collection Systems: Implementing robust systems for tracking health outcomes, participation rates, and community satisfaction is fundamental. Regularly reviewing this data helps in making timely adjustments.
- Setting Measurable Goals: Establishing clear, measurable goals lets communities identify what success looks like. For example, aiming for a 20% increase in health screenings within a year creates a tangible target.
- Public Reporting: Sharing progress with the community fosters transparency and trust. Publicly accessible reports on health improvements can encourage community members to engage with programs further.
By grounding strategies in data, from identifying disparities to monitoring outcomes, communities can better tackle health disparities and work toward health equity. Data-driven solutions not only empower those involved but also foster a culture of accountability and action, vital for sustainable change. Embracing this approach can bring about meaningful improvements in health outcomes for everyone.
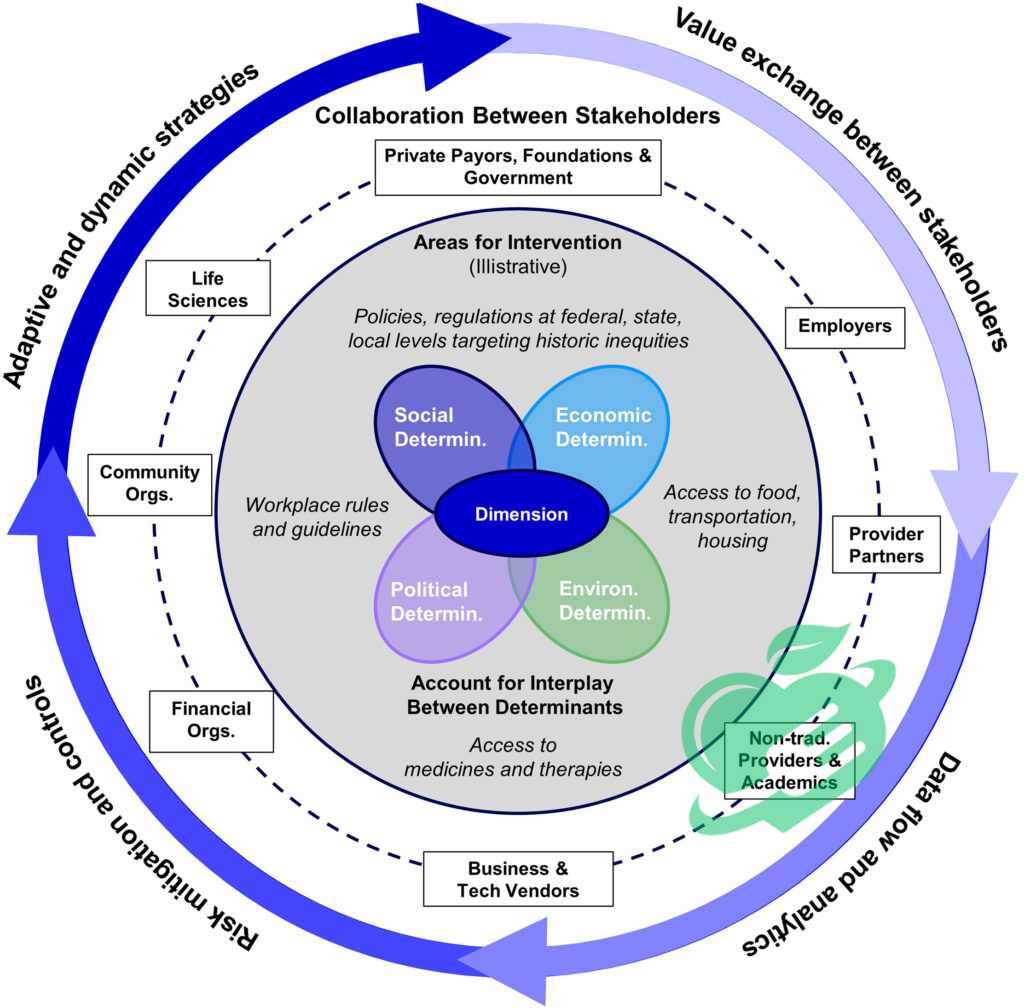
Collaborative Approaches for Sustainable Change
As we continue to address health disparities through data-driven solutions, the need for collaborative approaches becomes increasingly evident. Sustainable change doesn’t happen in isolation; it requires the collective efforts of various stakeholders, including healthcare providers, community organizations, and the individuals they serve.
Multi-sector Partnerships
Establishing multi-sector partnerships is foundational for tackling health disparities. By bringing together diverse organizations and sectors, we can pool resources and expertise to create robust solutions.
- Healthcare and Education: Collaborating with schools can help incorporate health education into curricula, empowering the next generation to prioritize their well-being. Programs that teach children about nutrition, physical activity, and mental health can create lasting change.
- Local Businesses and Health Initiatives: Engaging local businesses to promote health initiatives can be highly effective. For example, a local grocery store might offer discounts on healthy foods during a community health awareness month, promoting healthier eating habits.
- Government Agencies and Nonprofits: Partnerships between governmental agencies and nonprofits can lead to more comprehensive service delivery. By sharing data and insights, these partnerships can better address systemic barriers that contribute to health disparities.
Personal experiences shared by community leaders often emphasize that by collaborating across sectors, they have been able to maximize their impact, leading to improved health outcomes and community trust.
Health Disparities and Community Engagement
Community engagement is essential in ensuring that health interventions are relevant and successful. It’s crucial to include the voices of those most affected by health disparities in the decision-making process.
- Community Advisory Boards: Establishing boards made up of community members can provide invaluable insights into local needs and priorities. These boards can help shape health programs that genuinely resonate with the community.
- Participatory Research: Involving community members in research processes can enhance the relevance and effectiveness of health initiatives. Their lived experiences bring critical perspectives that can shape research questions and methods.
- Feedback Channels: Setting up easy-to-use feedback channels allows community members to share their thoughts on health services. Open forums, suggestion boxes, and digital surveys facilitate ongoing conversations, ensuring that health programs evolve with community needs.
Many community members find empowerment in their contributions, creating a sense of ownership over health initiatives, which in turn drives greater participation.
Read also: From Theory to Reality: Exploring the Feasibility of Blood Tests for Anxiety Disorders
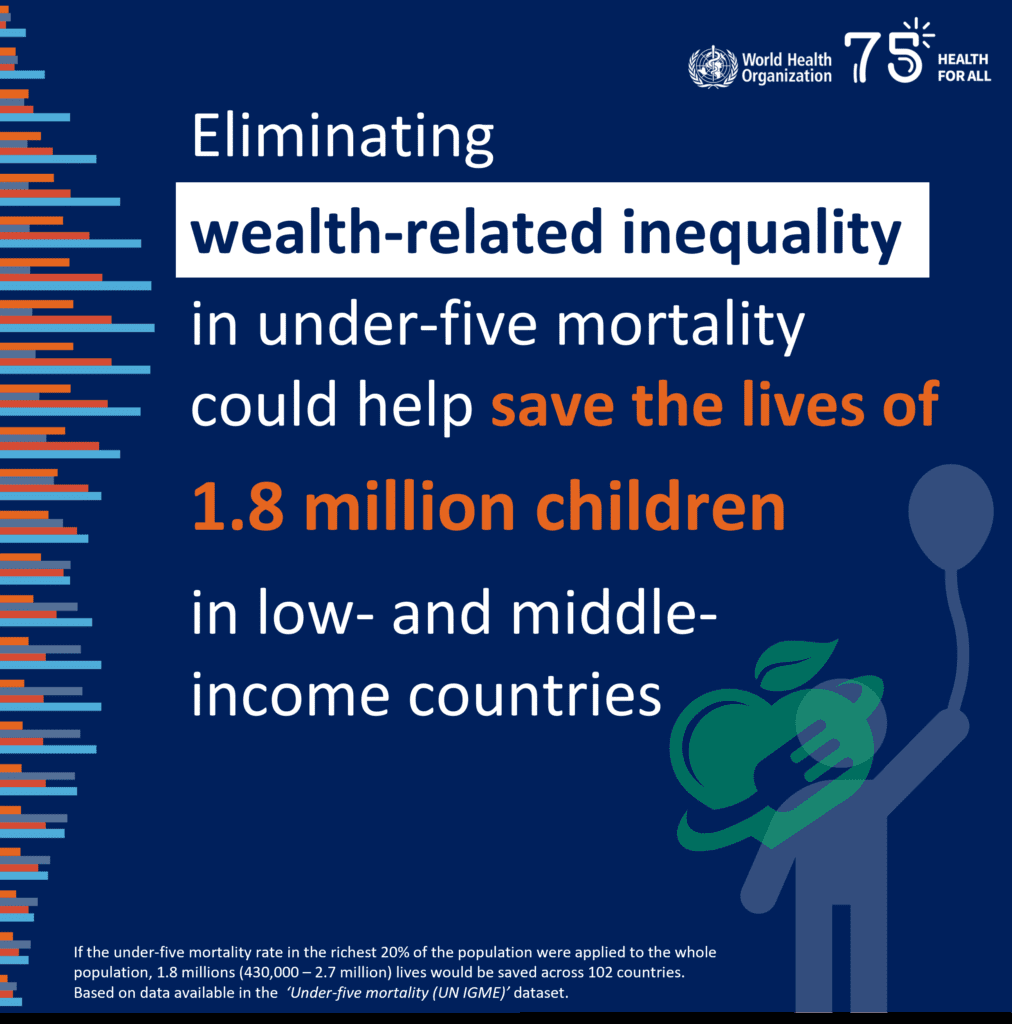
Empowering Marginalized Groups
Empowering marginalized groups is key to creating equitable health outcomes. Addressing the unique barriers they face will help foster an inclusive environment where everyone can thrive.
- Tailored Resources: Programs should be tailored to the specific needs of marginalized populations. For example, providing language assistance or culturally relevant resources can make healthcare more accessible for non-English speakers.
- Leadership Development: Investing in leadership training for individuals from marginalized groups can cultivate future healthcare advocates. When community members are equipped with skills and knowledge, they are better prepared to champion health equity initiatives.
- Advocacy Training: Teaching marginalized groups how to advocate for their health rights can lead to more significant systemic changes. Programs that empower individuals to engage with politicians and stakeholders strengthen community advocacy efforts.
In conclusion, collaborative approaches—through multi-sector partnerships, community engagement, and empowering marginalized groups—can lead to sustainable change in addressing health disparities. By working together and valuing diverse perspectives, we lay the groundwork for a healthier, more equitable future for all. These collective efforts strengthen communities and ensure that everyone has the opportunity to thrive.
Health Disparities: Future Directions in Health Equity
As we look to the horizon, several emerging trends promise to reshape the landscape of health equity. By leveraging advancements in technology, participating in global health initiatives, and aligning efforts with advocacy and sustainable development goals, we can make significant strides in creating equitable healthcare for all.
Technology Innovations
Technology is playing an increasingly critical role in bridging health disparities. Innovations are creating opportunities to enhance healthcare access and education:
- Telemedicine: The surge in telemedicine has transformed how individuals access care, especially in underserved areas. Imagine a rural resident who can consult a specialist located hundreds of miles away without the burden of travel costs. This service can greatly improve health outcomes for those who previously struggled to receive regular care.
- Health Apps: Mobile applications tailored for health monitoring have become game-changers. These apps enable users to track their health metrics easily, receive reminders for medications, and access educational resources. For instance, a community health app designed for the residents of San Bernardino could provide information in multiple languages, helping to ensure that diverse populations are informed and engaged.
- Data Analytics: Using big data analytics can provide insights into community health needs. By analyzing aggregated health data, organizations can identify trends and design targeted interventions that address specific gaps in care.
The excitement surrounding technology innovations stems from personal stories of individuals who have benefited from these advancements, leading to improved health management and stronger community connections.
Global Health Initiatives
Global health initiatives have gained momentum, fostering collaboration and knowledge-sharing across borders:
- Collaborative Research: Many organizations are now working together to research and tackle global health disparities. For example, information-sharing platforms enable health practitioners from various regions to exchange best practices tailored to their local contexts.
- Health Diplomacy: Countries are increasingly recognizing health as a common goal. Collaborative initiatives, such as vaccination drives or maternal health programs, enhance global solidarity and serve as a reminder that health knows no borders.
- Funding and Support: As global awareness of health disparities rises, funding for international health initiatives has made positive impacts. Local communities often thrive when equipped with additional resources to tackle their unique health challenges.
Personal stories of health workers traveling to support initiatives in low-resource settings underscore the importance of global health collaboration, revealing how interconnected our health truly is.
Advocacy on Health Disparities and the Sustainable Development Goals
Lastly, advocacy continues to drive the health equity conversation. Aligning local efforts with global sustainable development goals (SDGs) helps to create a unified framework:
- SDG 3 – Good Health and Well-Being: This goal emphasizes the importance of ensuring healthy lives for all. Local organizations can tailor their strategies to align with this overarching theme, emphasizing preventive care and accessibility.
- Community Involvement: Grassroots advocacy campaigns that empower individuals to take action are critical. For instance, community members can mobilize to advocate for policy changes aligned with SDGs, ensuring that their needs are prioritized.
- Collaboration with Policymakers: Building relationships with policymakers can amplify the voices of marginalized groups. Advocacy efforts focused on health equity can influence legislation, funding, and awareness campaigns to create systemic change.
Frequently asked questions
What is the best example of health disparity?
1) Mortality
Cancer serves as a prominent illustration of a significant cause of mortality that disproportionately impacts certain racial and ethnic demographics. African Americans experience the highest death rates from most cancers, even though their rates of developing the disease are lower compared to other racial and ethnic groups. 1.
What’s another word for health disparities?
These variations in health results are referred to as health inequalities – unjust and preventable disparities in health among the population and between various groups within society. 2.
What are disparities?
When you search for the term “disparity” in a dictionary, you will probably see it described as a difference, variation, or possibly inequality, without additional details. 3.
What is the best definition of health equity?
Health equity refers to the condition where all individuals have an equal and just chance to achieve their optimal health. 4.
Follow us for more updates and breaking news, as we provide you with everything new.