HIV Cure Breakthrough: What You Need to Know

Overview of HIV Cure Research
Historical Background of HIV/AIDS
The journey to understand and combat HIV/AIDS has been long and complex. Emerging in the early 1980s, the disease first garnered attention when rare infections and cancers began showing up among young gay men in the United States. This alarming trend quickly spread to other populations, forcing the medical community to confront a novel virus that presented unique challenges. The virus, Human Immunodeficiency Virus (HIV), was identified in 1983 by researchers at the Pasteur Institute and named shortly thereafter. By the mid-1980s, it became clear that HIV Cure is the causative agent of Acquired Immunodeficiency Syndrome (AIDS), which was characterized by the devastating effect it had on the immune system. Key historical milestones include:
- 1985: The first blood test for HIV was developed, allowing for early detection and improved screening in blood donations.
- 1996: The introduction of Highly Active Antiretroviral Therapy (HAART) revolutionized treatment, transforming HIV from a fatal diagnosis into a manageable chronic condition.
- 2000s: Understanding of the disease’s biology improved, leading to innovative treatment strategies that included pre-exposure prophylaxis (PrEP) and better patient care.
The stigma surrounding HIV/AIDS also played a significant role in shaping the response to the epidemic. Activist organizations, including ACT UP, took to the streets to demand better treatment options and funding, highlighting the intersection of politics and public health.
Current State of HIV Cure Research
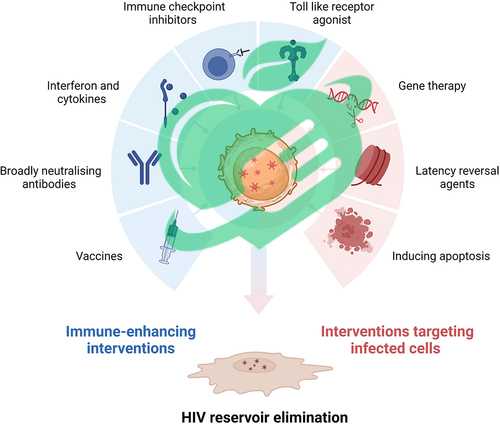
Today, the landscape of HIV cure research is more promising than ever before. Researchers are actively exploring various avenues to eradicate the virus from the body while balancing the need for effective treatments. This dual approach is crucial, as the current therapies primarily focus on managing the virus rather than eliminating it. Several avenues of research are currently being pursued:
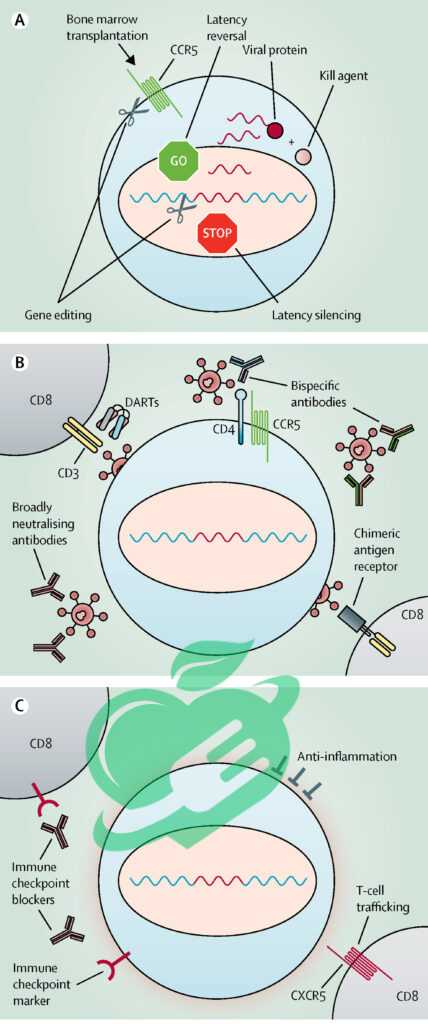
- Gene Editing: Techniques such as CRISPR/Cas9 are being utilized to target and disable the HIV genome within infected cells, potentially leading to a functional cure.
- Immunotherapy: Approaches like therapeutic vaccines are designed to boost the immune response to HIV, teaching the body to recognize and fight the virus more effectively.
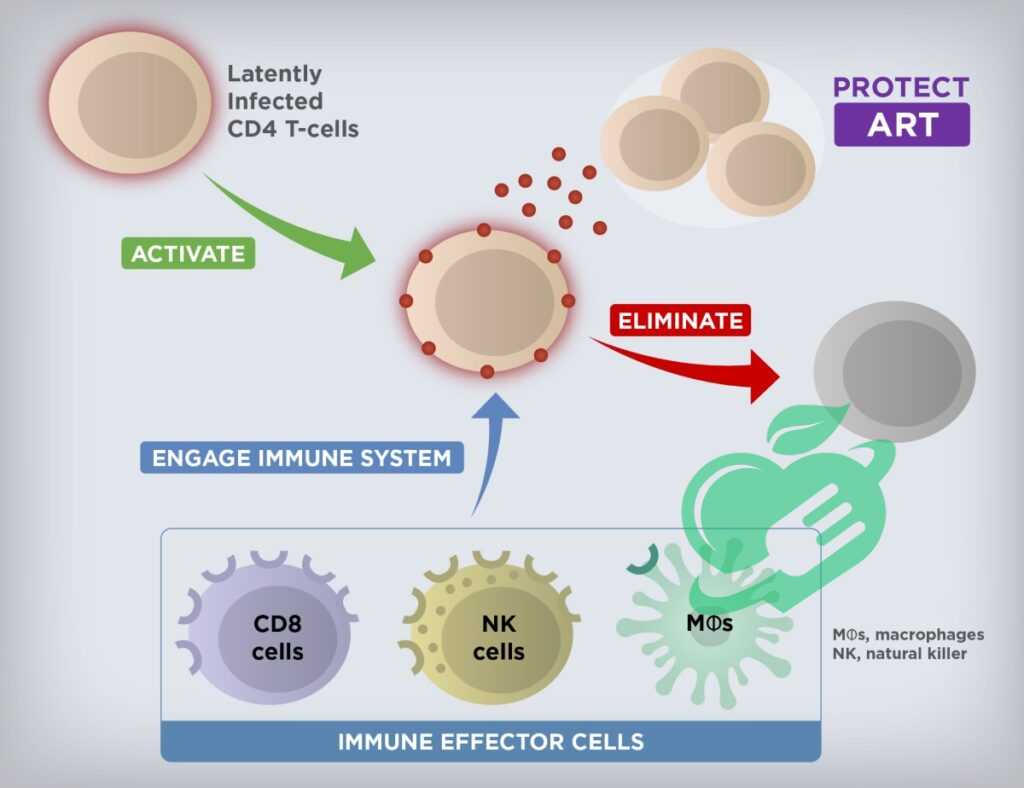
- Latency Reversal: Researchers are looking into ways to reactivate latent HIV reservoirs, encouraging the immune system to target and clear these hidden infections.
Significant progress has been observed, with a few individuals reported to be functionally cured through experimental treatments and stem cell transplants. However, these cases are rare and not yet applicable to broader populations. As the scientific community progresses towards an HIV cure, the collective hope remains that one day, the term “HIV positive” will fade, replaced by a world free of this virus. Continuous research, funding, and collaboration are vital to achieving this goal, moving beyond management and towards eradication.
Breaking Barriers in HIV Cure Development
Advances in Drug Therapies
As research into HIV cure development progresses, advances in drug therapies are playing a pivotal role in breaking down the barriers that have historically hindered treatment. The landscape of antiretroviral drugs has transformed significantly, with researchers continually seeking to enhance their efficacy while minimizing side effects. This advancement is not just about treating the virus, but also about paving the path toward a potential cure. Some notable advancements include:
- Long-Acting Injectables: Medications like cabotegravir and rilpivirine are now available in injectable forms, allowing patients to receive treatment every few months instead of daily pills. This innovation is particularly beneficial for those who struggle with adherence to oral medications.
- Broadly Neutralizing Antibodies (bNAbs): These engineered antibodies are designed to attack multiple strains of HIV, targeting the virus directly and potentially preventing its spread in the body. Early research has shown promise in their capability to lower viral loads effectively.
- Novel Drug Classes: New classes of antiretroviral drugs, such as integrase inhibitors and attachment inhibitors, are making waves in terms of their ability to disrupt the virus’s lifecycle. These drugs offer fresh options for treatment-experienced patients and can help maintain viral suppression.
The evolution of drug therapies has not only improved individual health outcomes but also redefined societal perceptions surrounding living with HIV. For many, managing HIV has transitioned from a daily struggle to a more routine aspect of life.
Read also : Breaking the Stigma: Real Genital Herpes Pictures Shared
Gene Editing Technologies in HIV Cure
Another groundbreaking avenue in HIV cure research involves gene editing technologies. One of the most talked-about innovations in this area is the CRISPR/Cas9 technique, which offers unprecedented precision in genetic modification. This revolutionary approach has opened new doors for eradicating HIV-infected cells. Here’s how gene editing is being leveraged in the fight against HIV:
- Targeting and Disabling HIV DNA: CRISPR can be designed to seek out and cut the specific DNA sequences of HIV integrated into the genome of infected cells. The goal is to remove or inactivate the virus, effectively reducing the viral load.
- Repairing Immune Cells: By editing the genes of immune cells, researchers are working to enhance the body’s natural defenses against HIV. This could revolutionize the way the immune system recognizes and combats infections.
- Preclinical Successes: There have been encouraging results from early studies in laboratory environments and animal models, showing that gene editing could lead to sustained viral remission in some cases.
A personal anecdote comes to mind about a researcher who, upon seeing the potential of gene editing, became driven to find a cure. His enthusiasm was infectious as he shared stories of patients who had regained hope through early trials. Despite the incredible potential of gene editing technologies, challenges still remain, including delivery mechanisms and ensuring safety. However, as scientists continue to refine these techniques, the horizon appears brighter for the possibility of a complete HIV cure. Through relentless innovation and persistence, both advances in drug therapies and gene editing technologies are proving to be powerful allies in the quest to eliminate HIV. The excitement in the research community is palpable, as they work collaboratively to transform hope into reality.
Challenges and Hurdles in Finding a Cure
Latent HIV Reservoirs
Despite the promising advancements in drug therapies and gene editing technologies, the journey towards an HIV cure is fraught with significant challenges. One of the most pressing hurdles is the existence of latent HIV reservoirs. Imagine a hidden fortress where the virus can lurk undetected, capable of re-emerging even after lengthy periods of antiretroviral treatment. Here’s how latent reservoirs pose a problem:
- Persistence of Reservoirs: HIV can integrate itself into the DNA of resting immune cells, effectively going underground. These latent reservoirs can be found in various parts of the body, including lymph nodes, the gut, and other tissues.
- Antiretroviral Therapy Limitations: Current treatments are excellent at managing viral loads in the bloodstream but cannot eliminate these hidden reservoirs. As a result, once therapy stops, the virus can rebound, creating an ongoing challenge for researchers.
- Reactivation Difficulty: Efforts to flush out dormant virus particles through strategies like latency-reversing agents offer potential, but they still need more optimization and efficacy. The delicate balance between activating the virus and not triggering an autoimmune response is critical.
One researcher shared a poignant story about a patient who had been living with HIV for years, successfully treated with antiretrovirals but grappling with the fear of potential viral rebound. This fear underscores the emotional burden that latent reservoirs impose on patients, making it clear that we cannot celebrate a cure until we address this challenge.
Immune System Evasion by HIV
Alongside the threat posed by latent reservoirs, HIV’s ability to evade the immune system is another significant barrier in the quest for a cure. This insidious virus has evolved tactics that allow it to stay one step ahead of the immune response, making it incredibly difficult to eradicate. Here’s how it accomplishes this:
- Rapid Mutation: HIV is notorious for its high mutation rate. With each replication, minor changes occur in its genetic material, which can help the virus escape detection by the immune system. This constant evolution means that even an effective immune response might only work against a limited number of virus variants.
- Downregulation of Immune Markers: HIV can alter the expression of proteins on the surface of infected cells. By downregulating CD4 receptors, which are crucial for identifying infected cells, the virus effectively camouflages itself from the immune system.
- Exploiting Immune Exhaustion: Chronic infection can lead to immune exhaustion, where T-cells (the body’s defenders) become less effective over time. This exhaustion allows HIV to persist in the body, thriving while the immune system struggles to mount a robust response.
One healthcare worker recounted the frustration of watching patients develop resistance to therapies due to these evasive maneuvers. It’s a heartbreaking reminder of the continuous cat-and-mouse game between HIV and the immune system. In conclusion, the path to an HIV cure is littered with challenges, primarily rooted in the complex interactions between the virus and the human immune system, along with the strategic survival tactics of this resilient virus. Addressing these challenges will require continued innovation and collaboration across the research landscape, reinforcing that the fight against HIV is far from over. The journey may be long, but the commitment to finding a cure remains unshaken.

Collaborative Efforts and Global Initiatives
International Partnerships in HIV Cure Research
Amid the myriad challenges faced in the quest for an HIV cure, a remarkable beacon of hope emerges through collaborative efforts and international partnerships. The complexity of HIV necessitates a team approach across various sectors, transcending geographical and disciplinary boundaries. Consider these key components facilitating international collaboration:
- Global Research Networks: Organizations such as the International AIDS Society (IAS) and the Global Fund to Fight AIDS, Tuberculosis and Malaria are central to fostering connections among researchers, clinicians, and public health officials worldwide. These networks provide a platform for sharing insights, resources, and innovative ideas.
- Public-Private Partnerships: Collaborations between academic institutions, pharmaceutical companies, and governmental organizations are crucial. For instance, the collaboration between Harvard University and Gilead Sciences to explore new therapeutic options illustrates how shared expertise can lead to accelerated discoveries.
- Global Conferences: Events like the International AIDS Conference serve as vital venues for knowledge exchange, where researchers present cutting-edge findings, and discuss strategies to overcome barriers to HIV research. These gatherings sow the seeds for future collaborations and inspire young scientists globally.
To illustrate the power of partnership, one researcher recounted her experience at an international conference where she formed connections that later led to a groundbreaking study on HIV latency. The relationships established at these events are invaluable, often translating into successful projects that push the boundaries of what we understand about HIV.
Funding and Support for HIV Cure Programs
Funding is the lifeblood of scientific progress, particularly in the realm of HIV cure research. The challenges of securing adequate financial resources can often make or break studies, and thus, various entities are stepping up to fill the gap. Here’s how funding is being leveraged:
- Government Grants: National Institutes of Health (NIH) and other governmental bodies provide substantial funding for innovative projects aimed at understanding and curing HIV. Researchers often apply for grants targeting specific issues, increasing their chances of securing support.
- Nonprofit Organizations and Foundations: Institutions like the Bill & Melinda Gates Foundation have made significant investments in HIV research, targeting specific goals like eradicating the virus in low-resource settings. Their support enables groundbreaking studies that might not receive funding from traditional sources.
- Crowdfunding and Grassroots Initiatives: In recent years, grassroots efforts have emerged, allowing communities and individuals to contribute to HIV research funding. These initiatives highlight the passion and commitment of ordinary people who believe in the importance of finding a cure.
A personal anecdote shared by a researcher highlights the impact of a modest crowdfunding effort that enabled her to conduct a pilot study investigating a new approach to HIV treatment. This grassroots funding not only catalyzed research but also fostered a sense of community commitment to the cause. In summary, collaborative efforts and robust funding mechanisms are essential drivers in the ongoing fight against HIV. By working together across borders and disciplines while securing necessary resources, the global community continues to shine a light on the path toward discovering an HIV cure. The journey may be fraught with challenges, but the ever-growing network of passionate individuals and organizations stands united in the belief that a future without HIV is not just a dream, but an achievable goal.
Ethical Considerations and Patient Perspectives
Ethical Issues in HIV Cure Trials
As the quest for an HIV cure advances, ethical considerations take center stage, especially when it comes to clinical trials. The urgency to find effective treatments must be balanced with the need to protect the rights and well-being of participants. Ethical dilemmas arise in various aspects of research, and it’s crucial to navigate these waters with care. Some pertinent ethical issues include:
- Informed Consent: Ensuring that participants fully understand the nature of the trial, its potential risks, and benefits is essential. This can be particularly challenging in populations that have historically faced stigmatization and discrimination. Researchers must communicate complex information in an accessible way, respecting the autonomy of individuals.
- Access to Trials: Often, marginalized communities may not have adequate access to cutting-edge HIV research studies. This raises concerns about equity and whether certain groups are unfairly excluded from benefiting from new advancements.
- Risk vs. Benefit Analysis: With experimental treatments involved, researchers must carefully weigh the potential risks against the expected benefits to participants. For some, the fear of adverse effects may lead to reluctance in participating, underscoring the importance of transparency throughout the process.
Read also : Unraveling the Mystery: Common Triggers of Painful Urination
A poignant example comes from a participant in an HIV cure trial who spoke about her experience. After expressing her hope for a cure, she discovered how crucial informed consent was, as it empowered her to make informed decisions about her health. Her story serves as a reminder of the importance of viewing participants as partners in the research process.
Patient Involvement and Advocacy
Involving patients in HIV cure research not only enriches the scientific process but also empowers those living with the virus. Patient advocacy is a powerful force in shaping research priorities and improving the relevance of studies to real-world challenges. Here are some key aspects of patient involvement:
- Advocacy Organizations: Groups such as the Treatment Action Group (TAG) and local community organizations play significant roles in amplifying patient voices. They advocate for increased funding, equitable access to trials, and a seat at the table for those directly affected by the virus.
- Feedback on Research Design: Engaging patients in the design of clinical trials can lead to invaluable insights. Their lived experiences can inform researchers about critical factors, such as what side effects matter most or how to improve recruitment strategies.
- Peer Support Networks: Many patients find solace and strength in connecting with others facing similar challenges. These networks not only provide emotional support but also create a platform for collective advocacy efforts pushing for more ethical and effective research.
A former HIV activist shared a personal anecdote about how participating in advocacy efforts led to significant changes in trial protocols. By voicing their concerns, patients ensured increased safety measures and support during trials, demonstrating the power of collective action. In conclusion, ethical considerations and patient perspectives play crucial roles in the landscape of HIV cure research. By prioritizing ethical standards in trials and actively involving patients, researchers can foster a culture of respect and trust. Ultimately, the collaborative efforts between scientists and communities can pave the way for a future where effective treatments and, hopefully, a cure for HIV are within reach. The journey is complex, but together, we can adhere to shared values and work toward achieving equitable outcomes for all.

Future Prospects and Emerging Trends
Promising Approaches in HIV Cure
As researchers forge ahead in the fight against HIV, several promising approaches are emerging on the horizon, igniting hope for an eventual cure. These innovative strategies harness a combination of science, technology, and community input, reflecting the multifaceted nature of HIV research. Here are some of the most exciting developments:
- Therapeutic Vaccines: Unlike preventive vaccines, therapeutic vaccines aim to stimulate an immune response in those already infected with HIV. Trials are underway to evaluate several candidates, with the hope that they can help control the virus without lifelong therapy.
- Gene Therapy and Editing: Advances in gene editing technologies, particularly CRISPR/Cas9, are paving the way for eradicating HIV from infected cells. Ongoing studies aim to refine these techniques to ensure they effectively target HIV without unintentionally affecting other parts of the genome.
- Shock and Kill Strategies: This approach attempts to flush out latent HIV reservoirs by “shocking” dormant virus particles and then employing therapies to eliminate them. While challenging, early trials show promise in manipulating the latent reservoirs while keeping the immune system intact.
- Broadly Neutralizing Antibodies (bNAbs): By targeting multiple strains of HIV simultaneously, bNAbs may offer a novel treatment approach by neutralizing the virus or preventing it from establishing infections. Researchers are working on creating more effective versions derived from individuals with robust immune responses.
A researcher’s story about a patient who participated in a therapeutic vaccine trial stands out. That patient experienced a significant reduction in viral load, illustrating the hope these experimental treatments bring to the community. As we advance in these approaches, each step brings us closer to a potential cure.
Potential Timelines for Achieving an HIV Cure
While the progress in HIV research is encouraging, predicting a specific timeline for achieving a cure remains elusive. The complexity of HIV and the various strategies being explored necessitate cautious optimism rather than definitive timelines. Here are some considerations impacting timelines:
- Ongoing Research Outcomes: As each trial provides insights, researchers may need additional time to analyze results, refine protocols, and conduct further studies. Each field’s progression depends heavily on what discoveries are made in current efforts.
- Regulatory Frameworks: The approval process for new therapies can be lengthy, requiring rigorous testing to ensure safety and efficacy. While expedited pathways exist for promising treatments, the timeline can still be unpredictable.
- Funding and Resources: Adequate funding is vital. With continued financial support from public and private organizations, researchers can expedite trials and broaden their scope, potentially shortening the timeline for breakthrough discoveries.
As an activist once shared at a community meeting, even though exact timelines are difficult to pin down, the sense of urgency felt by those living with HIV fuels dedication in research. There’s an unmistakable optimism in the air. In summary, future prospects for an HIV cure hinge on innovative approaches and collaborative efforts rooted in patient involvement. The scientific community is diligently pursuing groundbreaking strategies that hold the promise of delivering transformative outcomes. While timelines remain uncertain, the unwavering commitment to find a cure reflects a community united in the hope that one day, the phrase “living with HIV” will evolve into “living free from HIV.” As each day passes, researchers strive to transform this hope into reality, one significant advance at a time.



