Understanding Meningitis and Its Link to Headaches
Overview of Meningitis
meningitis and headache-is a serious infection that causes inflammation of the protective membranes covering the brain and spinal cord. Understanding this condition is crucial for early detection and treatment, as timely intervention can be life-saving.
Definition and Types-meningitis and headache
Meningitis and headache can manifest in various forms, each caused by different pathogens. It’s primarily classified into two main types:
- Viral Meningitis: This is the most common type and is usually less severe. Viruses such as enteroviruses, herpes simplex virus, and mumps virus are common culprits. Most people recover fully with adequate hydration and rest.
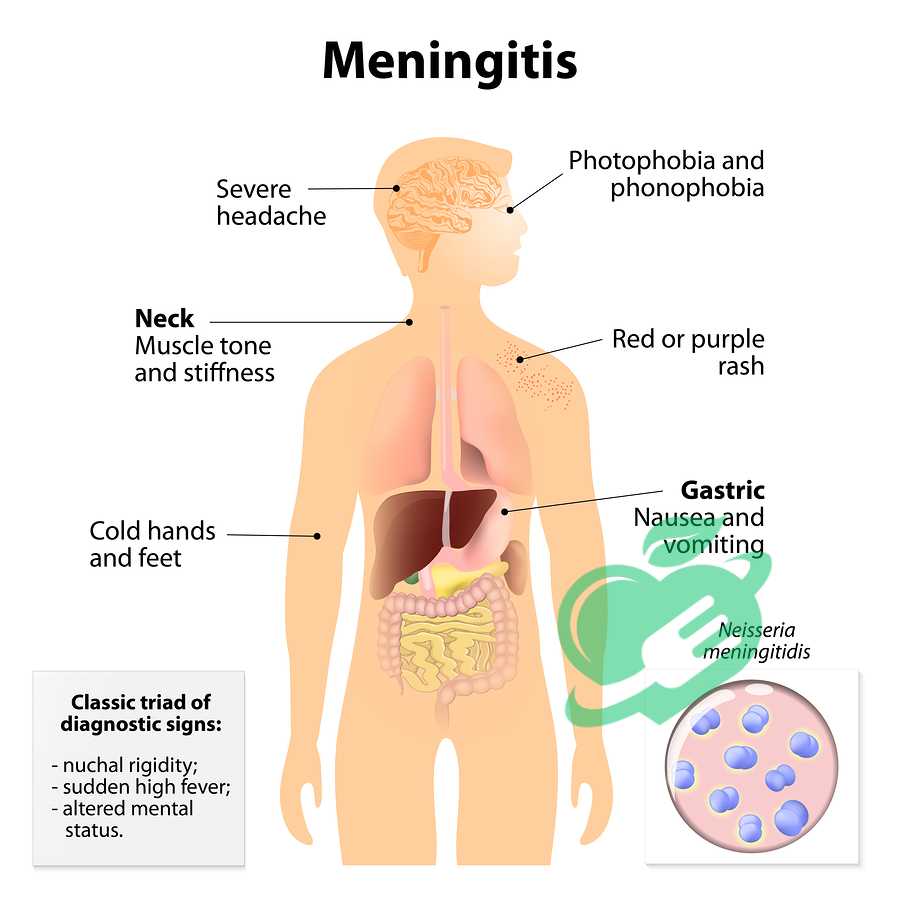
- Bacterial Meningitis: This is more severe and can lead to serious complications or death if not treated promptly. The bacteria that most frequently cause bacterial meningitis include Neisseria meningitidis, Streptococcus pneumoniae, and Haemophilus influenzae. This type often requires immediate medical attention, including hospitalization and antibiotics.
- Fungal Meningitis: Although rarer, this form can be serious, particularly in individuals with weakened immune systems. It’s often caused by fungal infections that spread to the brain.
Understanding the type of meningitis is essential for determining the appropriate treatment protocol.
Causes and Risk Factors
Meningitis arises from various infectious agents or, less commonly, non-infectious factors. Some common causes include:
- Infections: As discussed above, viruses and bacteria are the primary infective agents. Additionally, less common causes like fungi and parasites can also result in meningitis.
- Physical Injury: A skull fracture or other injury that affects the head can increase the risk of bacterial meningitis.
- Medical Conditions: Conditions such as HIV, diabetes, and certain cancers can weaken the immune system, making individuals more susceptible to infections.
Risk factors associated with meningitis include:
- Age: Infants and young children are at higher risk of viral meningitis, while adolescents and young adults are more susceptible to bacterial meningitis.
- Living Arrangements: Crowded living conditions, such as dormitories, can facilitate the spread of bacteria, increasing risk.
- Travel: Traveling to countries where certain types of meningitis are more common can heighten exposure to pathogens.
- Certain Medical Procedures: Procedures that involve the spinal cord or brain may increase the risk of infection.
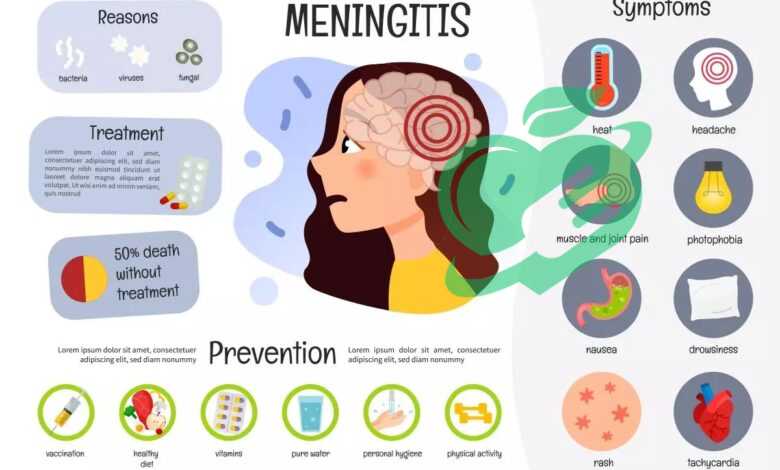
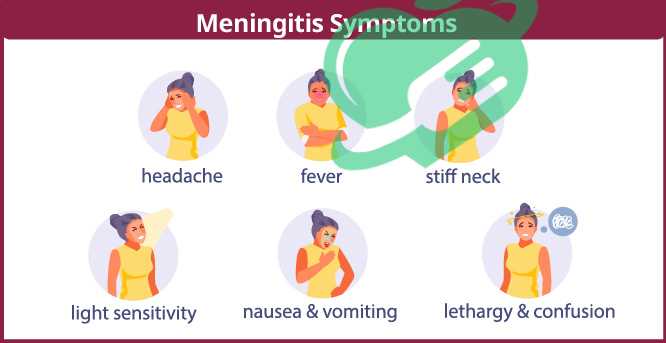
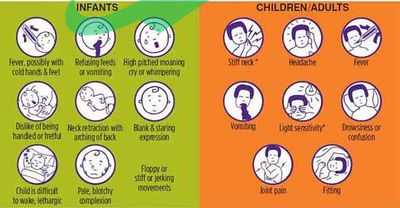
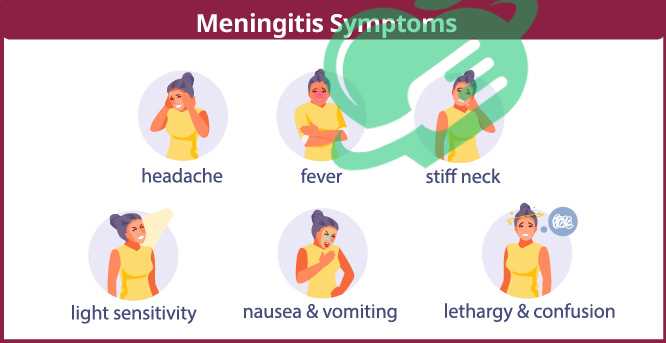
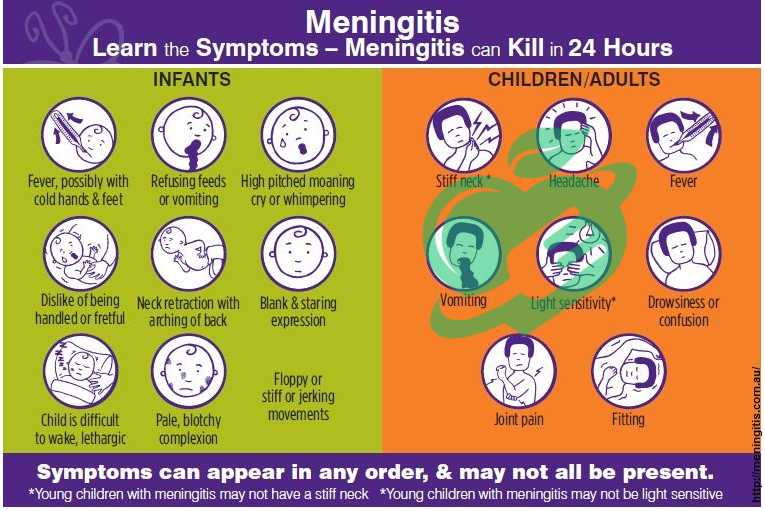
Symptoms and Warning Signs-meningitis and headache
Recognizing the symptoms of meningitis early is vital. Common signs and symptoms include:
- Fever: Often one of the first indicators.
- Severe headache: A headache that feels different from any previous headaches.
- Stiff neck: Difficulty touching chin to chest can signal meningitis.
- Sensitivity to light: Bright lights may cause discomfort.
- Nausea or vomiting: Accompanied by other symptoms.
On top of these, there may be other warning signs to observe, especially in young children:
- Irritability or confusion: Changes in behavior.
- Rash: A rash that does not fade when pressed could indicate meningococcal meningitis.
It’s essential to seek medical attention if these symptoms appear, as early diagnosis can lead to better outcomes.
Read also: From Theory to Reality: Exploring the Feasibility of Blood Tests for Anxiety Disorders
Understanding Headaches in Meningitis
As we delve deeper into meningitis, one of the hallmark symptoms that stands out is the headache. This isn’t just any headache; it is often one of the most debilitating aspects of the illness. Understanding this connection is essential for recognizing the disease early.
How Headaches are Linked to Meningitis-meningitis and headache
Headaches associated with meningitis are a result of inflammation and irritation of the membranes surrounding the brain and spinal cord. When the meninges—the layers of tissue protecting the brain—become inflamed due to infection, this triggers pain in multiple areas. Here’s how the headache typically manifests:
- Intensity: Meningitis headaches are often severe and pulsating. They can feel like a constant pressure or an intense throbbing, which doesn’t relent easily.
- Location: Unlike tension headaches that might feel tight across the forehead, meningitis headaches can radiate throughout the head. Many describe a “band-like” pressure around the skull.
- Accompanied Symptoms: These headaches rarely appear in isolation. They usually accompany other symptoms like fever, nausea, and a stiff neck. The combination of these symptoms can be telling.
For example, when one of my friends experienced severe headaches along with a stiff neck and high fever, it was a concerning combination that prompted immediate medical attention. This proved crucial, as it ultimately led to a quick diagnosis of viral meningitis.
Differentiating Meningitis Headaches from Other Types
Not all headaches are created equal, and distinguishing a meningitis headache from other types can be life-saving. Here are key differences that can help identify a meningitis headache:
- Duration: Meningitis headaches tend to be persistent and may last for days, whereas tension-type headaches often fluctuate in intensity and can come and go.
- Response to Medication: Over-the-counter pain relievers like ibuprofen or acetaminophen may alleviate tension headaches but are typically less effective against the throbbing intensity of a meningitis headache.
- Associated Symptoms: The combination of fever, neck stiffness, sensitivity to light, and nausea is often absent in other types of headaches. If you experience a headache along with these symptoms, it’s crucial to seek medical advice.
- Onset: Meningitis headaches can develop rapidly over a few hours or a day, leaving the individual feeling overwhelmed. In contrast, migraines often build up and include visual disturbances or aura preceding the headache.
In summary, understanding the unique characteristics of headaches associated with meningitis is vital for early recognition of the infection. If a headache comes with other alarming symptoms, it’s better to act quickly rather than wait and see. Your health is worth the precaution!
Diagnosis of Meningitis
Identifying meningitis quickly can be a matter of life and death. The diagnostic process is crucial for determining the presence of the infection and initiating appropriate treatment.
Medical History and Physical Examination-meningitis and headache
The journey to diagnosing meningitis typically begins with a thorough medical history. The healthcare provider will ask detailed questions to understand the patient’s symptoms and health background. Key areas of focus include:
- Symptom Onset: When did the headache, fever, and other symptoms start?
- Recent Illnesses: Have there been any recent infections, hospitalizations, or vaccinations?
- Travel History: Did you travel somewhere with a known outbreak of meningitis?
- Exposure Risks: Have you been in contact with anyone diagnosed with meningitis or showed similar symptoms?
During the physical examination, the healthcare provider will look for classic signs of meningitis:
- Neck Stiffness: Patients may exhibit resistance to neck movements, particularly trying to touch their chin to their chest.
- Rash: A petechial or purpuric rash may indicate bacterial meningitis, particularly meningococcal meningitis.
- Neurological Symptoms: Assessing mental status, including confusion or drowsiness, can provide vital information.
Just last year, a family friend was misdiagnosed with a severe migraine after presenting with a headache and fever. It wasn’t until they conducted a thorough physical check that the stiff neck was considered, leading to a timely diagnosis of meningitis.
Tests and Procedures for Confirming Meningitis-meningitis and headache
If meningitis is suspected, further testing is essential to confirm the diagnosis. Following a comprehensive exam, the healthcare provider may recommend several tests:
- Lumbar Puncture (Spinal Tap): This is the most definitive test for meningitis. By extracting cerebrospinal fluid (CSF), doctors can analyze it for bacteria or viruses. It’s crucial for identifying the type of meningitis correctly.
- Blood Tests: These can reveal signs of infection and help in identifying which organism is responsible for the illness, whether it’s viral or bacterial.
- Imaging Tests: In some cases, CT or MRI scans might be ordered to look for swelling or other complications in the brain. This helps rule out other conditions that may present similar symptoms.
- PCR Testing: This test on CSF or blood can identify specific viral pathogens providing additional insights into the type of meningitis.
Ultimately, a combination of these examinations and tests will lead to a decisive diagnosis. The importance of swift diagnosis cannot be overstated, as the outcome often hinges on how quickly the right treatment is administered. In any scenario where meningitis is suspected, never hesitate to seek immediate medical advice. Every moment counts!
Read also: Sinus Headache SOS: Quick Fixes and Long-Term Solutions
Treatment Options for Meningitis
Once diagnosed, the next critical step is determining the appropriate treatment for meningitis. Treatment options vary based on the type of infection, whether it’s bacterial or viral, emphasizing the need for timely intervention.
Antibiotics and Antiviral Medications – Meningitis and Headache-meningitis and headache
For bacterial meningitis, the first line of defense is usually a powerful course of antibiotics. These medications are typically administered intravenously to ensure they reach the bloodstream quickly, tackling the infection head-on. Here’s what to expect:
- Types of Antibiotics: Common choices include ceftriaxone, vancomycin, or ampicillin, selected based on the identified bacteria.
- Prompt Administration: Time is of the essence; as soon as bacterial meningitis is suspected, antibiotics should start immediately, even before lab results come back.
On the other hand, viral meningitis often resolves on its own, which means antiviral medications aren’t typically prescribed. However, in certain severe cases, such as those caused by the herpes simplex virus, antivirals like acyclovir may be indicated to reduce the duration and severity of symptoms. A few years ago, a relative experienced sudden onset headaches and fever, leading to a diagnosis of bacterial meningitis. Thanks to rapid treatment with antibiotics, they made a remarkable recovery. This experience highlighted the critical importance of early intervention in improving outcomes.
Supportive Care and Hospitalization-meningitis and headache
Supportive care is an essential component of managing meningitis, regardless of whether it’s viral or bacterial. Here’s what supportive treatment often encompasses:
- Hospitalization: Due to the severity of meningitis, most patients are hospitalized for close monitoring and treatment. This is particularly vital for bacterial meningitis, where a patient’s condition can deteriorate rapidly.
- Fluid Management: Maintaining hydration is crucial. IV fluids help manage hydration levels, which is significant during fever and illness.
- Pain Management: Severe headaches and neck pain often accompany meningitis. Healthcare providers typically provide pain relief through medications tailored to the patient’s specific needs.
- Monitoring Neurological Status: Regular assessments of the patient’s mental and neurological state help identify any changes that could indicate complications.
- Gradual Return to Activities: Once discharged, patients are usually advised to ease back into their daily routines, particularly as headaches may continue for some time.
It’s important to remember that while supportive care significantly aids recovery, the journey doesn’t end after leaving the hospital. Regular follow-ups with healthcare providers will ensure a safe and complete recovery, addressing any lingering concerns or complications. In conclusion, treatment options for meningitis are diverse and need to be tailored to the individual patient’s needs. Rapid recognition and intervention play pivotal roles in improving outcomes, underscoring the importance of awareness about this serious condition.
Complications and Long-Term Effects-meningitis and headache
While prompt diagnosis and treatment of meningitis can lead to full recovery, it is essential to recognize that complications may still arise. Being informed about potential risks and the necessity for follow-up care can significantly aid in managing long-term health.
Potential Risks Associated with Meningitis-meningitis and headache
Meningitis can leave lasting effects or potentially lead to severe complications. Some of the risks you might encounter include:
- Neurological Damage: This is one of the most concerning complications. Inflammation can lead to issues such as memory problems, cognitive deficits, or difficulty concentrating. Some may even experience seizures.
- Hearing Loss: Particularly with bacterial meningitis, hearing impairment can occur due to the infection affecting the auditory nerves. It’s vital to monitor hearing post-recovery.
- Learning Disabilities: Children who have experienced meningitis are sometimes at risk of developing learning difficulties or delays in their educational progress.
- Gait and Motor Skills Issues: Some individuals may find that they experience coordination difficulties, affecting their balance or motor skills.
- Infections and Other Health Issues: Surviving meningitis doesn’t guarantee freedom from health issues. Complications can lead to other infections, chronic fatigue, or immune system challenges.
A family friend shared their experience of battling through bacterial meningitis. While they managed to recover quite well physically, they faced ongoing challenges with short-term memory and fatigue that required adjustments in their daily life.
Rehabilitation and Follow-Up Care-meningitis and headache
Rehabilitation plays a crucial role in the recovery journey for those affected by meningitis. Here’s what follow-up care often entails:
- Regular Medical Check-ups: Following discharge from the hospital, continual visits to healthcare providers are essential to assess for any lingering complications. Regular screenings for hearing loss and cognitive evaluation might be included.
- Physical and Occupational Therapy: If coordination and motor skills are affected, therapy can significantly help regain strength and function. Tailored exercises can assist with balance and muscle strength.
- Counseling and Behavioral Therapy: Emotional support is paramount. Individuals may feel anxious or depressed as they navigate a new reality after meningitis. Therapy can help process these feelings and build resilience.
- Education Support for Children: Should children face learning disabilities, special education services might be necessary to provide them with the tools they need to succeed.
- Support Groups: Connecting with others who have had similar experiences can foster understanding and provide practical coping strategies.
Ultimately, while the road to recovery from meningitis can be challenging, with appropriate follow-up care and rehabilitation, many individuals can regain fulfilling and active lives. Awareness of potential complications and proactive management can make a significant difference in one’s long-term health.
Read also: Brain Freeze Buster: Remedies for Instant Relief
Prevention Strategies
Preventing meningitis is essential, not only for individual health but also for community well-being. By being proactive, we can significantly reduce the risk of infection. Here are the key strategies to consider.
Vaccination Recommendations-meningitis and headache
Vaccines play a pivotal role in protecting against various types of meningitis. It’s crucial to be informed about which vaccines are available and recommended for different age groups. Here’s an overview:
- Meningococcal Vaccines: These vaccines protect against Neisseria meningitidis, a leading cause of bacterial meningitis. Typically recommended for:
- Preteens (11-12 years old) and teenagers (around 16 years old).
- College students residing in dormitories.
- Individuals with certain medical conditions.
- Pneumococcal Vaccines: Protecting against Streptococcus pneumoniae, which can lead to both pneumonia and meningitis, these are recommended for:
- Infants and young children (PCV13) and older adults (PPSV23).
- Individuals with weakened immune systems.
- Haemophilus Influenzae Type B (Hib) Vaccine: This vaccine is typically given to infants and toddlers to guard against infections that can lead to meningitis.
- Varicella and Mumps Vaccines: These vaccines help prevent infections that can result in viral meningitis.
When my cousin’s child turned one, she ensured he received his vaccines on schedule. A few years later, she learned that her diligence had helped protect him against several serious infections, including meningitis. Staying updated with vaccinations not only protects yourself but also helps foster herd immunity, critical for those who cannot be vaccinated due to medical reasons.
Hygiene Practices to Prevent Meningitis-meningitis and headache
Aside from vaccinations, implementing good hygiene practices can significantly help mitigate the risk of contracting meningitis. Here are some actionable tips:
- Frequent Hand Washing: Regularly washing hands with soap and water, especially after using the restroom, before eating, or after being in public spaces, is incredibly effective in stopping the spread of germs.
- Avoid Sharing Personal Items: Shared drinking glasses, utensils, and personal hygiene items like toothbrushes can transmit infections. Encourage kids to respect personal belongings.
- Maintain Good Respiratory Hygiene: Covering coughs and sneezes with a tissue or sleeve helps prevent the spread of respiratory droplets.
- Stay Away from Sick Individuals: If someone has a cold or flu-like symptoms, it’s wise to limit close contact until they recover.
- Clean Surfaces Regularly: Regularly disinfecting frequently-touched surfaces at home and in shared spaces can help reduce the spread of bacteria and viruses.
- Practice Safe Food Handling: Ensuring food is stored and prepared correctly can prevent gastrointestinal infections that could lead to a higher susceptibility to meningitis.
embracing both vaccination and hygiene best practices forms a comprehensive strategy for preventing meningitis. It’s a responsibility we all share to protect not only ourselves but those around us. By prioritizing these preventative measures, we can contribute to a healthier community for everyone.