Cardiomyopathy Ischemic ICD 10: What You Need to Know
Overview of Cardiomyopathy Ischemic ICD 10
Definition and Meaning of Ischemic Cardiomyopathy
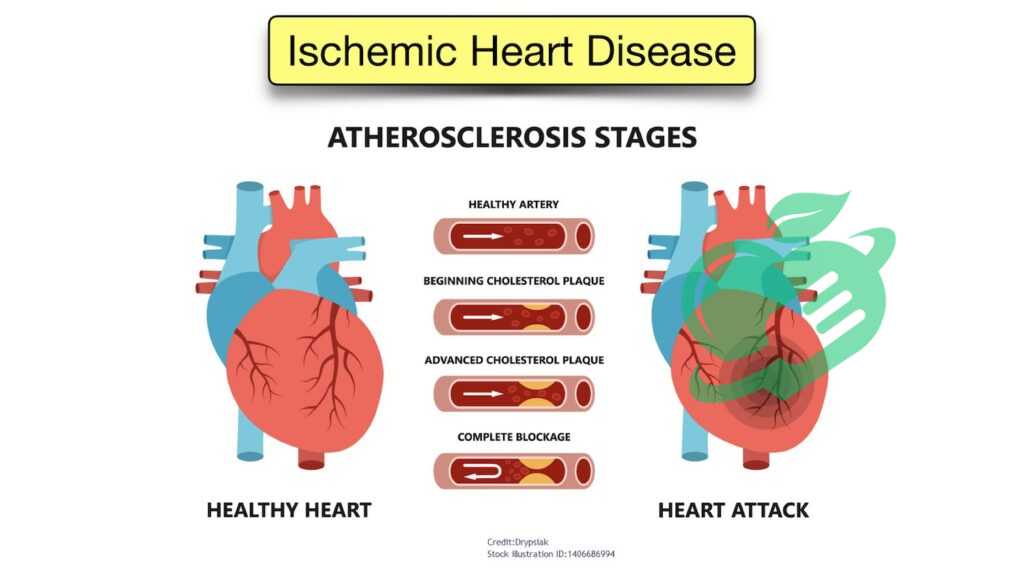
Cardiomyopathy Ischemic ICD 10 is a condition that arises when the heart muscle becomes weak due to insufficient blood supply, typically linked to coronary artery disease. When the coronary arteries are narrowed or blocked, the heart muscles do not receive enough oxygen and nutrients, which can lead to damage over time. This condition can be particularly concerning for those with risk factors such as high blood pressure, high cholesterol, or a family history of heart diseases. To put it into perspective, imagine taking a road trip and encountering unexpected roadblocks along the way. Just as a roadblock hinders your progress, narrowed arteries obstruct blood flow to the heart, leading to symptoms like fatigue, shortness of breath, and even chest pain. Ischemic cardiomyopathy may develop gradually, and individuals might not realize they are experiencing heart strain until the symptoms become pronounced or they face heart failure complications.
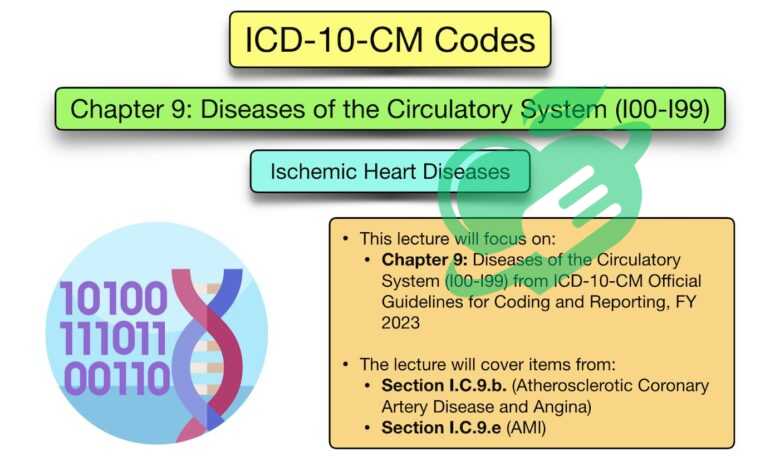
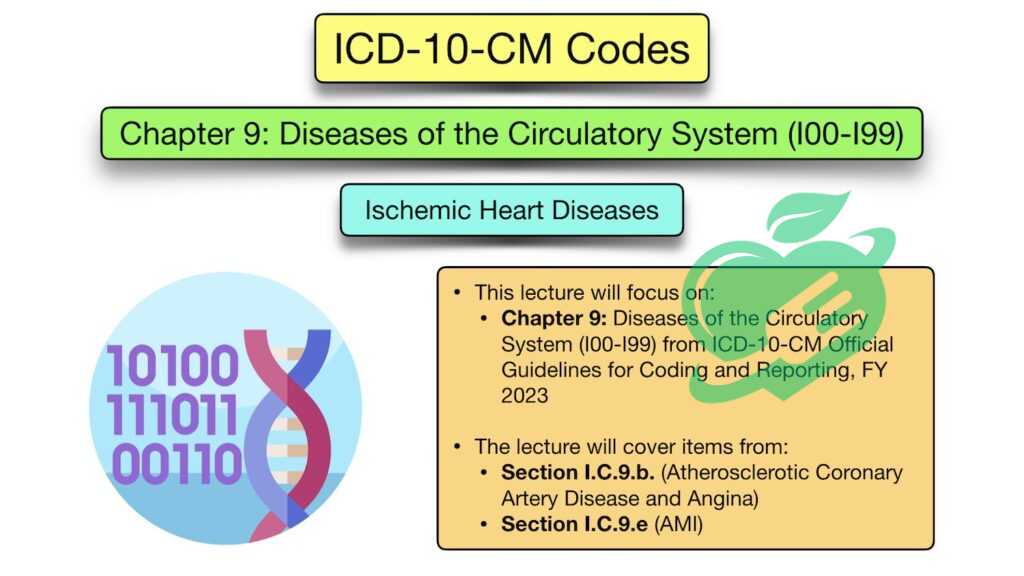
Introduction to Cardiomyopathy Ischemic Icd 10 Coding System
The ICD-10 (International Classification of Diseases, 10th Revision) coding system plays a crucial role in the healthcare industry, providing a standard way to document and categorize health conditions. Ischemic cardiomyopathy has a specific code that allows healthcare professionals to communicate about the condition efficiently, essential for treatment planning, insurance reimbursement, and disease tracking. Here’s a quick overview of the significance of the ICD-10 coding system:
- Standardization: It creates a universal language for healthcare providers across different regions and facilities.
- Accurate Billing: Correct coding helps ensure healthcare providers are reimbursed accurately for the services rendered.
- Statistical Analysis: The data collected through ICD-10 codes contributes to public health statistics and can influence policies and funding.
In essence, understanding both ischemic cardiomyopathy and its coding under the ICD-10 system is vital for both patients and healthcare providers, ensuring appropriate care and relevant administrative processes.

Causes and Risk Factors
Common Causes of Ischemic Cardiomyopathy
Ischemic cardiomyopathy is primarily caused by a prolonged reduction in blood flow to the heart muscle, often due to various forms of coronary artery disease. Understanding these causes can provide insight into how to prevent or manage this condition effectively. Here are some common causes:
- Coronary Artery Disease (CAD): This is the most common cause, characterized by the buildup of plaque in the coronary arteries, which restricts blood flow.
- Myocardial Infarction: Heart attacks can lead to permanent damage to the heart muscle, resulting in ischemic cardiomyopathy as the heart struggles to pump blood efficiently.
- Severe Anemia: When the body lacks adequate red blood cells, the heart may not receive enough oxygen-rich blood, putting it under strain.
- Prolonged High Blood Pressure: Chronic hypertension can thicken and weaken the heart muscle over time.
Personal stories often help illustrate these causes. For instance, a friend of mine had a family history of heart disease but ignored his hypertension for years. Eventually, this led to a heart attack, followed by the diagnosis of ischemic cardiomyopathy.
Risk Factors Associated with Ischemic Cardiomyopathy
Identifying risk factors can be crucial for prevention. Here’s a list of risk factors that significantly contribute to ischemic cardiomyopathy:
- Age: Risk increases with age, particularly for men over 45 and women over 55.
- Family History: A genetic predisposition to heart diseases can heighten risk.
- Smoking: Tobacco use damages blood vessels and contributes to plaque buildup.
- Obesity: Excess weight puts strain on the heart and can lead to conditions like diabetes.
- Diabetes: Poorly controlled blood sugar levels can damage blood vessels, promoting heart disease.
- Sedentary Lifestyle: Lack of physical activity greatly increases the risk of heart problems.
Being aware of these causes and risk factors can empower individuals to take proactive steps to prioritize their heart health. Early intervention and lifestyle changes can make a significant difference in preventing ischemic cardiomyopathy.
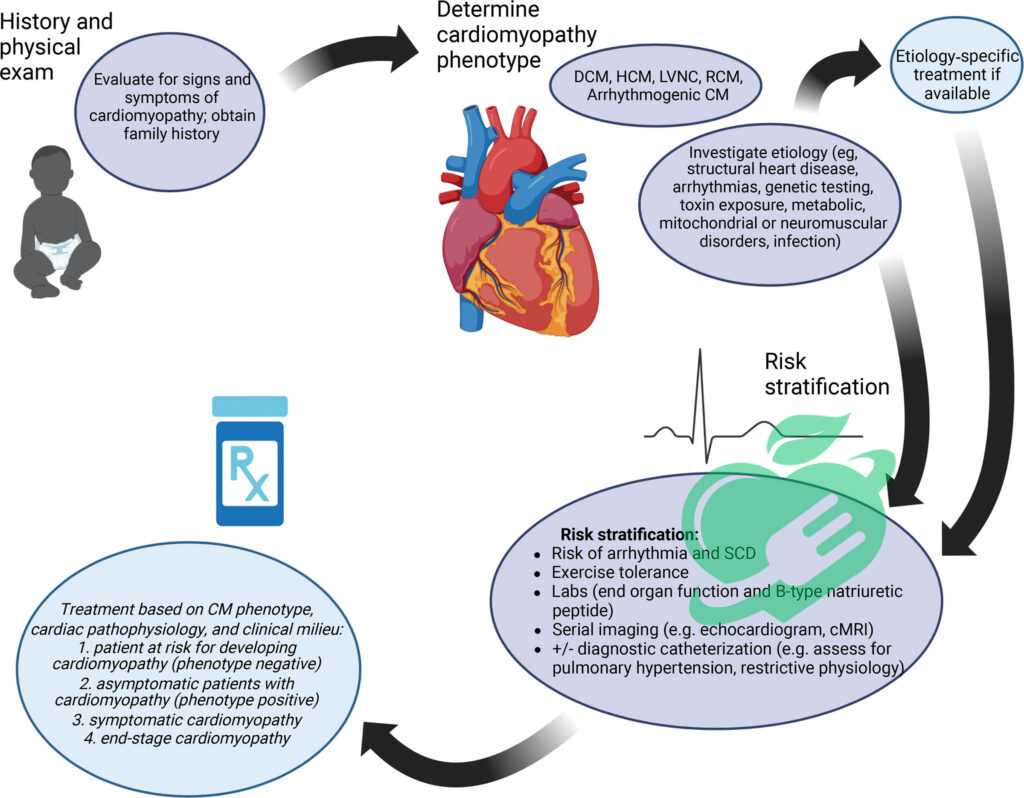
Symptoms and Diagnosis
Signs and Symptoms of Ischemic Cardiomyopathy
Recognizing the signs and symptoms of ischemic cardiomyopathy is vital for early intervention. Individuals may experience a range of symptoms, some of which can be subtle at first. Here are the most common signs to look out for:
- Shortness of Breath: Often occurs during physical activity or even at rest in advanced cases.
- Fatigue: A general feeling of exhaustion can be a significant warning sign, particularly with minimal exertion.
- Chest Pain or Discomfort: This may feel like pressure, squeezing, or aching in the chest, often worsened by activity or stress.
- Lightheadedness or Dizziness: Experiencing these symptoms can indicate reduced blood flow to the brain.
- Swelling: Accumulation of fluid in the legs, ankles, or abdomen may accompany heart problems.
An anecdote comes to mind about a colleague who brushed off her persistent fatigue as just the result of a busy lifestyle. It wasn’t until she experienced severe shortness of breath while walking her dog that she realized it was time to seek help.
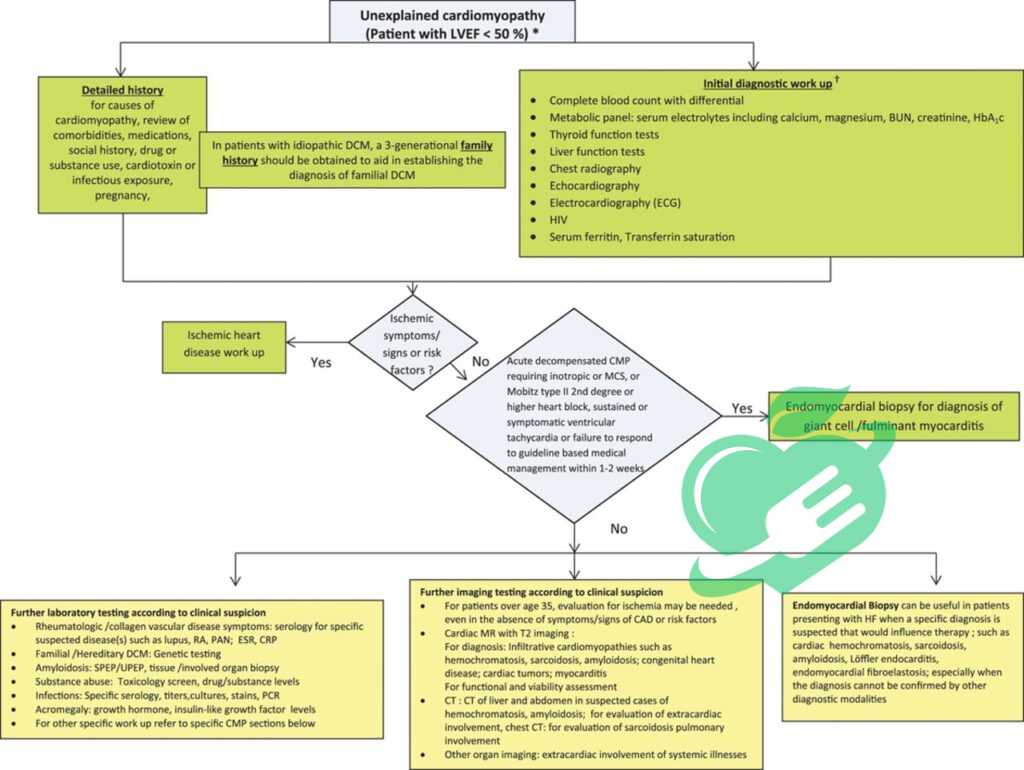
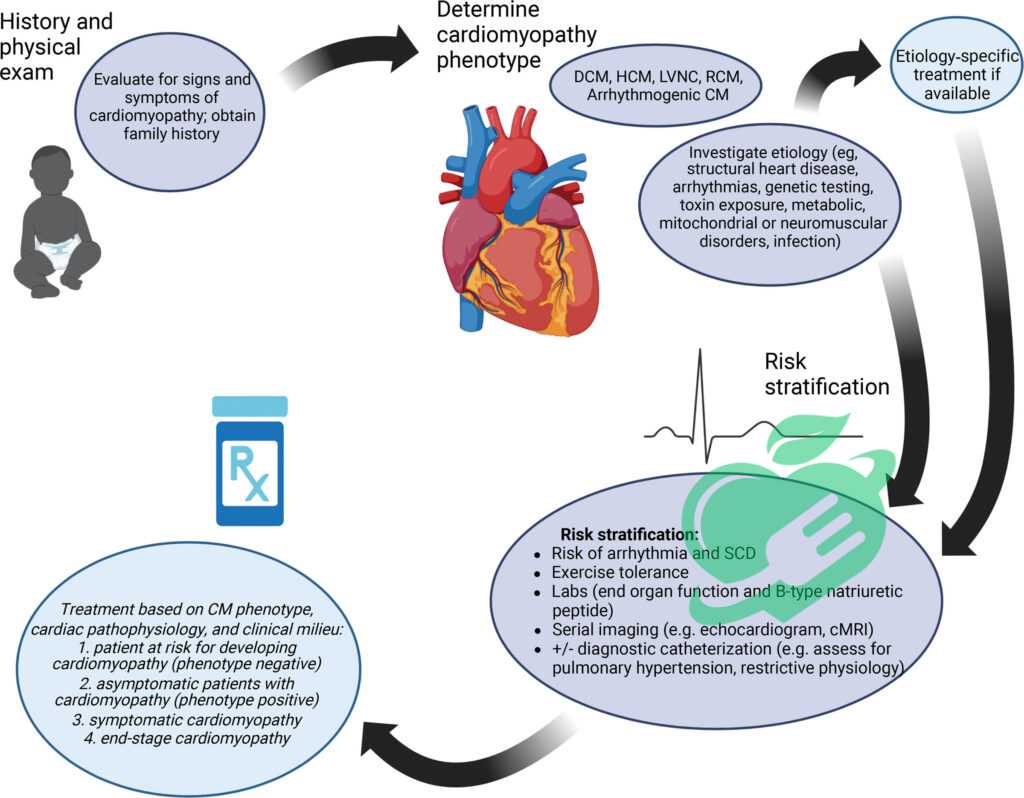
Diagnostic Procedures and Tests for Ischemic Cardiomyopathy
If ischemic cardiomyopathy is suspected, a healthcare provider will recommend various diagnostic procedures to assess heart function and blood flow. These tests may include:
- Electrocardiogram (ECG): Measures the electrical activity of the heart and can identify irregularities.
- Echocardiogram: Aultrasound test that provides images of the heart, showing how well it pumps blood.
- Stress Test: Evaluates the heart’s performance under physical exertion, often involving exercise on a treadmill.
- Coronary Angiography: A minimally invasive procedure where contrast dye is injected into the coronary arteries to visualize blockages via X-ray.
- Blood Tests: These can help measure markers like troponin, which may indicate heart muscle damage.
Understanding these symptoms and the diagnostic process can empower individuals to take control of their heart health. The sooner ischemic cardiomyopathy is diagnosed, the more effective the treatment options can be.
Read also : Understanding Meningitis and Its Link to Headaches
Treatment Options – Cardiomyopathy Ischemic Icd 10
Medications for Ischemic Cardiomyopathy
When diagnosed with ischemic cardiomyopathy, many patients may feel overwhelmed, but there are effective treatment options available. Medications play a crucial role in managing the condition and can help alleviate symptoms, improve heart function, and reduce the risk of further complications. Here are the primary types of medications often prescribed:
- ACE Inhibitors: These help relax blood vessels, reducing the workload on the heart and improving blood flow.
- Beta-Blockers: They slow down the heart rate and lower blood pressure, which can help lessen the heart’s strain.
- Diuretics: Known as “water pills,” diuretics help remove excess fluid from the body, reducing symptoms of swelling and shortness of breath.
- Anticoagulants: These medications thin the blood, lowering the risk of blood clots, which can lead to strokes or heart attacks.
For example, a friend of mine was prescribed a combination of ACE inhibitors and beta-blockers after his diagnosis. Over time, he noticed significant improvements in his ability to engage in daily activities without feeling exhausted.
Surgical Interventions and Therapies
In more severe cases where medications are not sufficient, surgical interventions may be needed. Several options are available depending on the individual’s specific needs:
- Coronary Angioplasty and Stenting: This procedure opens up narrowed or blocked coronary arteries, often using a balloon for dilation and a stent to keep the artery open.
- Coronary Bypass Surgery: In this surgery, arteries or veins from other parts of the body are used to bypass blocked coronary arteries, restoring healthy blood flow to the heart muscle.
- Implantable Cardioverter-Defibrillator (ICD): For those at high risk for life-threatening arrhythmias, an ICD can be implanted to monitor heart rhythms and deliver shocks if needed.
- Heart Transplant: In cases of extreme heart failure where other treatments have failed, a heart transplant may be considered as a last resort.
Understanding these treatment options helps patients and their families navigate life with ischemic cardiomyopathy more effectively. Early and appropriate care can lead to better outcomes and improve quality of life significantly.
Prognosis and Complications – Cardiomyopathy Ischemic Icd 10
Prognosis of Ischemic Cardiomyopathy
The prognosis for patients diagnosed with ischemic cardiomyopathy can vary significantly based on several factors, including the level of heart damage, the underlying causes, and how early treatment is initiated. Generally, early detection and appropriate management can lead to improved outcomes. Here are some key points regarding prognosis:
- Improvement with Treatment: Many patients experience a stabilization or even improvement in heart function with effective medication and lifestyle changes.
- Survival Rates: Studies suggest that patients with mild to moderate ischemic cardiomyopathy can have survival rates that mirror those without heart problems, especially with proactive management.
- Monitoring is Key: Regular follow-ups and adherence to medications can greatly enhance quality of life and longevity.
A close friend’s father was diagnosed with ischemic cardiomyopathy but, with dedication to treatments and a heart-healthy lifestyle, he has been able to enjoy his life actively, enjoying his grandchildren and hobbies well into his seventies.
Potential Complications and Long-Term Effects
While the prognosis can be encouraging, patients with ischemic cardiomyopathy are at risk for several complications that can impact overall health. Here are some potential complications and long-term effects:
- Heart Failure: As the heart muscle weakens, it may struggle to pump blood effectively, leading to congestive heart failure.
- Arrhythmias: Irregular heartbeats can potentially lead to serious health issues, including sudden cardiac arrest.
- Cardiogenic Shock: This condition occurs when the heart fails to pump enough blood to meet the body’s needs, becoming a life-threatening emergency.
- Increased Risk of Heart Attacks: Patients may remain at risk for future heart attacks, particularly if lifestyle changes aren’t made.
Understanding the prognosis and potential complications allows patients and families to set realistic expectations and engage in proactive management. Open communication with healthcare providers about symptoms and lifestyle changes is vital for keeping the heart healthy and mitigating risks, ensuring that individuals can lead fulfilling lives despite their diagnosis.
Prevention and Management
Lifestyle Modifications for Prevention – Cardiomyopathy Ischemic Icd 10
Prevention plays a critical role in managing ischemic cardiomyopathy and ensuring a healthier future. Making conscious lifestyle modifications can significantly reduce the risk factors that contribute to heart disease. Here are some key lifestyle changes to consider:
- Balanced Diet: Eating heart-healthy foods is crucial. Incorporate:
- Fruits and vegetables
- Whole grains
- Lean proteins like fish and poultry
- Healthy fats such as olive oil and avocados
- Regular Exercise: Aim for at least 150 minutes of moderate aerobic activity weekly. Activities such as walking, swimming, or cycling can help strengthen the heart and improve circulation.
- Quit Smoking: If you smoke, seek resources to help quit. Smoking significantly increases the risk of heart complications.
- Weight Management: Maintaining a healthy weight reduces strain on the heart. Small changes, such as portion control and mindful eating, can make a big difference.
A personal story that resonates with many is when a friend transformed her diet after her spouse’s heart attack. By adopting a Mediterranean diet and committing to daily walks, they both noticed improvements in their overall health and energy levels.
Strategies for Managing Ischemic Cardiomyopathy
Once diagnosed, managing ischemic cardiomyopathy becomes essential to maintaining heart health. Here are effective management strategies:
- Medications Adherence: Regularly take prescribed medications. Establishing a routine or using pill organizers can help ensure consistency.
- Regular Monitoring: Schedule routine check-ups with healthcare providers to monitor heart function and any changes in symptoms.
- Stress Management: Engage in relaxation techniques such as yoga, meditation, or deep breathing exercises. Stress can negatively impact heart health, so finding ways to unwind is crucial.
- Educate Yourself: Understanding ischemic cardiomyopathy empowers patients to make informed decisions. Participate in support groups or educational programs to stay updated on new research or treatment options.
By implementing these lifestyle modifications and management strategies, individuals can significantly enhance their quality of life and take control of their heart health. Commitment to these changes not only benefits the heart but promotes overall well-being, allowing individuals to lead fulfilling lives despite their diagnosis.
Cardiomyopathy Ischemic Icd 10 Coding and Documentation
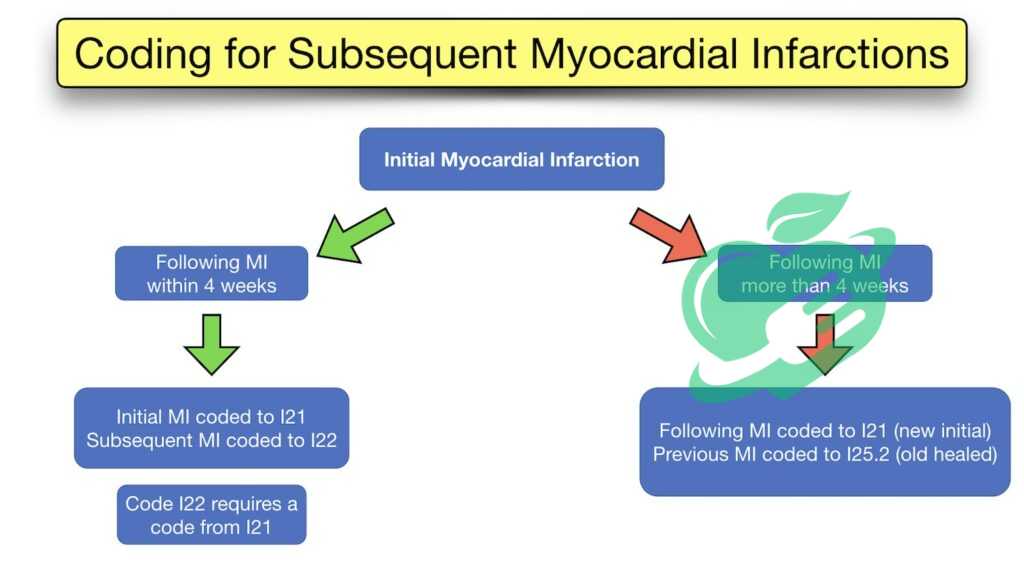
Coding Guidelines for Ischemic Cardiomyopathy
Accurate coding is essential for effectively managing ischemic cardiomyopathy cases, ensuring that patients receive appropriate treatment and that healthcare providers are reimbursed accordingly. The ICD-10 coding system includes specific codes designated for ischemic cardiomyopathy, which healthcare providers must be familiar with. Here are the key coding guidelines to keep in mind:
- ICD-10 Code: Ischemic cardiomyopathy is most commonly coded as I25.5.
- Specificity: Healthcare providers must select the correct code based on the specific circumstances of each patient’s condition. This helps avoid generalizations that could lead to improper treatment plans.
- Documentation Relevance: It’s important to document all relevant clinical findings and the progression of the disease. This includes noting any additional risk factors such as hypertension or prior myocardial infarctions.
During my time volunteering at a local health clinic, I observed how meticulously the staff maintained coding accuracy, which directly impacted patient care and treatment approvals.
Read also : Is POTS Disease Hereditary? Find Out the Truth!
Importance of Accurate Documentation
Accurate documentation and coding go hand in hand. Good documentation practices are crucial not only for coding purposes but also for ensuring high-quality patient care. Here’s why accurate documentation is important:
- Continuity of Care: Maintaining detailed records about a patient’s diagnosis, treatment, and progress allows all healthcare professionals involved to stay informed, ensuring consistent care.
- Quality Control: Accurate documentation is essential for healthcare audits and quality improvement initiatives. It helps identify patterns or discrepancies in patient care.
- Billing and Reimbursement: Misleading or incorrect documentation can lead to claim denials, impacting the financial health of the medical practice.
- Legal Protection: In the case of disputes or legal challenges, thorough documentation serves as a protective measure for healthcare providers.
In summary, understanding the coding guidelines and the significance of accurate documentation helps foster a more efficient healthcare system, ultimately leading to better patient outcomes in managing ischemic cardiomyopathy. By being diligent in these aspects, healthcare professionals can support their patients more effectively and provide them with the highest standard of care.
Resources and Support – Cardiomyopathy Ischemic Icd 10
Supportive Resources for Individuals with Ischemic Cardiomyopathy
For those living with ischemic cardiomyopathy, finding the right resources and support can have a profound impact on both emotional and physical well-being. Many patients benefit from a variety of supportive resources that can provide information, encouragement, and community engagement. Here are some helpful resources to consider:
- Educational Materials: Numerous websites and healthcare organizations offer brochures, articles, and online materials focusing on the management of ischemic cardiomyopathy, emphasizing heart-healthy habits.
- Support Groups: Local or online support groups can connect individuals with similar experiences. Sharing stories and coping strategies can provide comfort and reduce feelings of isolation. Websites like Meetup and Facebook often have groups dedicated to heart health.
- Counseling Services: Talking with a mental health professional can help manage the emotional burden of a chronic illness. Many patients find that therapy can contribute to a positive outlook and better coping strategies.
A friend of mine, diagnosed with ischemic cardiomyopathy, found immense value in an online support group, where he could share his journey and learn from others facing similar challenges.
Read also : Empowering Your Health Journey with an Endocrinologist’s Care
Organizations Offering Help and Information – Cardiomyopathy Ischemic Icd 10
Several organizations are dedicated to providing support and resources for individuals living with ischemic cardiomyopathy and other heart conditions. Some notable organizations include:
- American Heart Association (AHA): The AHA offers a wealth of resources, including educational materials, research findings, and guidelines for heart health.
- Heart Failure Society of America (HFSA): HFSA focuses specifically on heart failure and provides patients with tools and resources to manage their condition more effectively.
- National Heart, Lung, and Blood Institute (NHLBI): This organization provides comprehensive information about various heart diseases, including ischemic cardiomyopathy, research updates, and living well with heart disease.
- Shannon’s Heart Foundation: This nonprofit focuses on raising awareness and providing resources for patients with heart disease. They host community events and provide educational scholarships for patients.
Accessing these supportive resources and organizations can empower individuals living with ischemic cardiomyopathy to take control of their health journey, foster connections with others, and ultimately lead healthier and more fulfilling lives. Engaging with these resources can make a significant difference in navigating the complexities of heart health.