Diabetic Retinopathy ICD 10 Coding Made Simple
Overview of Diabetic Retinopathy
Diabetic Retinopathy ICD 10 Coding Made Simple is a serious eye condition that affects individuals living with diabetes. Understanding this condition is essential for both patients and healthcare providers, as early detection can significantly alter outcomes.
Definition of Diabetic Retinopathy
Diabetic retinopathy is a complication of diabetes that results from damage to the blood vessels of the retina, the light-sensitive tissue at the back of the eye. This damage can lead to vision loss and, in severe cases, blindness. It typically develops in stages, with the condition initially being asymptomatic and progressing over time if not adequately managed. The retina relies on a rich blood supply to function properly, and high blood sugar levels can cause changes that weaken and leak tiny blood vessels in this area. These changes can manifest in two main types of diabetic retinopathy:
- Non-Proliferative Diabetic Retinopathy (NPDR): In this early stage, the blood vessels in the retina become swollen or leak, leading to the formation of microaneurysms. NPDR can progress to more serious stages if blood sugar levels remain uncontrolled.
- Proliferative Diabetic Retinopathy (PDR): This is the advanced stage of the disease where new, abnormal blood vessels grow on the surface of the retina or into the vitreous gel of the eye. These vessels are fragile and prone to bleeding, which can lead to severe vision problems. 1.
Read also: Unlocking the Benefits: How Veggies Can Lower Your Blood Pressure.
Causes and Risk Factors
Several factors contribute to the development of diabetic retinopathy, primarily linked to uncontrolled diabetes. Here are some of the most significant causes and risk factors:
- Duration of Diabetes: The longer a person has diabetes, the higher the risk for developing DR. After about 10 years of diabetes, over 50% of individuals may experience some form of retinopathy.
- Poor Blood Sugar Control: Consistently high blood sugar (glucose) levels can damage blood vessels, leading to the onset and progression of DR.
- High Blood Pressure: Hypertension can exacerbate blood vessel damage in the eyes, significantly increasing the risk of DR.
- High Cholesterol Levels: Elevated cholesterol can contribute to blood vessel problems, making the eyes susceptible to retinopathy.
- Smoking: This habit can impair blood flow and oxygen supply to the retinas, compounding the effects of diabetes.
- Pregnancy: Pregnant women with diabetes may experience a faster progression of diabetic retinopathy.
- Genetics: Family history may also influence the risk of developing diabetic retinopathy. 2.
Symptoms and Progression
In its early stages, diabetic retinopathy often has no noticeable symptoms. Patients may not realize they have a problem until the condition has progressed. As it advances, individuals might experience various symptoms, which can include:
- Blurred or distorted vision
- Dark or empty areas in the vision
- Difficulty seeing at night
- Loss of central vision
- Sudden vision changes, such as flashes of light or floaters
The progression of diabetic retinopathy typically follows a pattern:
- Mild Non-Proliferative Retinopathy: Small lesions called microaneurysms appear, but vision may still be unaffected.
- Moderate Non-Proliferative Retinopathy: Symptoms can start to become noticeable as more significant blood vessel changes occur.
- Severe Non-Proliferative Retinopathy: Many blood vessels are blocked, threatening the blood supply to the retina.
- Proliferative Retinopathy: New, abnormal vessels form, leading to a higher risk of serious vision impairment.
To put things into perspective, Sarah, a 35-year-old woman diagnosed with type 1 diabetes at age 12, thought she was doing everything right by keeping her blood sugar levels under control. However, during a routine eye exam, her optometrist detected early signs of diabetic retinopathy despite her efforts. This experience underscored for her the importance of regular screenings and diligent diabetes management to prevent potential complications like blindness. By understanding the definition, causes, and symptomatology of diabetic retinopathy, individuals with diabetes can better navigate their health management and engage with their healthcare providers to safeguard their vision. Regular monitoring and preventive strategies are vital in addressing this serious condition.
Read also: Cardiomyopathy Ischemic ICD 10: What You Need to Know.
ICD-10 Codes for Diabetic Retinopathy
After understanding the complexities of diabetic retinopathy, it’s essential to delve into how this condition is classified in the healthcare system. The International Classification of Diseases, Tenth Revision (ICD-10), serves as a standardized system that clinicians and health providers use to code various diseases and health conditions, including diabetic retinopathy.
Understanding Diabetic Retinopathy ICD 10 Coding System
The ICD-10 coding system was established to provide a universal language for diagnosing and reporting conditions. This system is crucial for several reasons:
- Standardization: It ensures that medical professionals across the globe use the same codes and language, making it easier to share patient records.
- Billing and Reimbursement: Accurate coding is fundamental for appropriate billing practices. Insurers require specific ICD-10 codes to determine coverage.
- Data Tracking: Public health organizations use these codes to track disease prevalence, healthcare access, and health disparities, guiding future research and resource allocation.
What’s noteworthy about the ICD-10 coding system is its complexity and specificity. Each code corresponds to a particular diagnosis and may include additional characters to indicate various details about the condition, such as severity or laterality (right or left eye). For instance, diabetic retinopathy has unique codes that identify its different types and stages, which we will explore next.
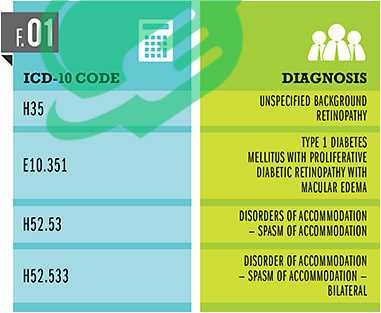
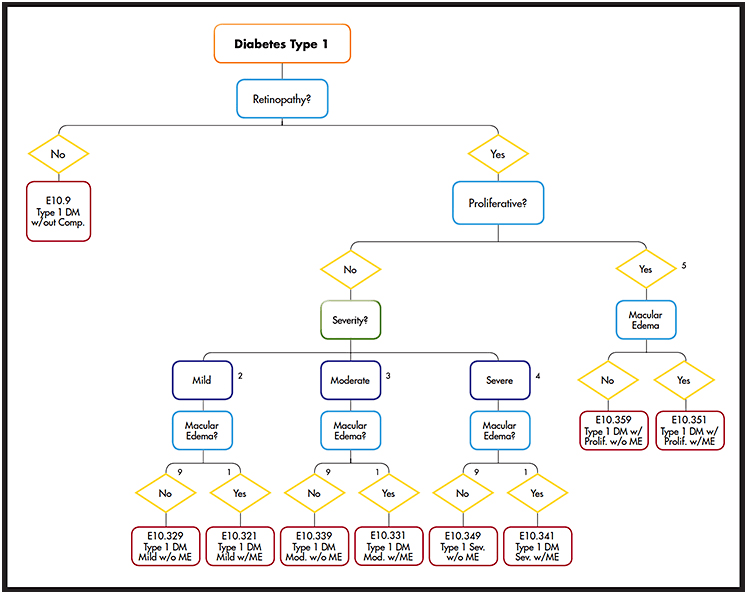
Specific Codes for Different Types and Stages
When it comes to diabetic retinopathy, the ICD-10 codes are particularly detailed. Let’s look at the codes that make up this crucial classification:
- E11.359: Other specified diabetic retinopathy with macular edema (without mention of the stage).
- E11.3591: Nonproliferative diabetic retinopathy with macular edema.
- E11.3592: Proliferative diabetic retinopathy with macular edema.
- E11.3593: Nonproliferative diabetic retinopathy without macular edema, stages unspecified.
- E11.367: Unspecified diabetic retinopathy, stage unspecified.
Understanding these codes can significantly impact patient care. For example, when John, a diabetic patient, was referred to an ophthalmologist for suspected diabetic retinopathy, the specialist used the ICD-10 code E11.359. This code indicated progression and provided the necessary information to assess not just the scope of John’s condition but also to streamline his treatment plan effectively. Here’s a breakdown to summarize:
| ICD-10 Code | Description |
|---|---|
| E11.359 | Other specified diabetic retinopathy, unspecified |
| E11.3591 | Proliferative diabetic retinopathy,with macular edema |
| E11.3592 | Nonproliferative diabetic retinopathy without macular edema |
| E11.3593 | Proliferative diabetic retinopathy with macular edema |
| E11.367 | Unspecified diabetic retinopathy, unspecified |
the condition’s severity and complications,
These specific codes provide clarity regarding the condition’s severity and complications, allowing healthcare providers to offer tailored care based on an individual’s needs. The knowledge of ICD-10 coding can empower patients, as understanding their diagnosis code may promote better conversations with their healthcare providers. It can serve as a tool for patients to ask more informed questions regarding their condition and treatment options. As patients like John navigate their journey with diabetic retinopathy, awareness of how their condition is coded can foster a greater understanding of their health and ensure they receive appropriate and timely care. Being proactive and informed can lead to better management of their diabetes and its complications. Understanding these codes not only deepens the knowledge about the disease but also enhances the connection patients have with their medical care.

Diagnosis and screening of diabetic retinopathy ICD 10
Having explored the coding system for diabetic retinopathy, it’s essential to pivot toward assessing how this condition is diagnosed and the significance of timely screening. Early detection is critical in managing diabetic retinopathy and maintaining overall eye health, as it can make a tremendous difference in preventing vision loss.
Read also: Understanding the New Diabetes Criteria: What You Need to Know
Importance of Early Detection
Imagine being unaware that a silent threat is lurking in your body—this is often the case with diabetic retinopathy. Many individuals may not experience noticeable symptoms in the early stages. According to the American Academy of Ophthalmology, about 80% of people with diabetes will develop some form of diabetic retinopathy after 15 years of living with the disease. This fact highlights the urgency of regular eye examinations. The benefits of early detection include:
- Preventing Vision Loss: Identifying DR in its early stages allows for timely intervention, which can prevent significant vision impairment or blindness.
- Personalized Treatment Plans: Early diagnosis enables healthcare providers to develop tailored plans that fit the individual’s specific needs and circumstances.
- Monitoring Progression: Regular screenings help track changes in the eyes and provide insight into how effectively the diabetes is being managed. 3.
Take Sarah, for instance, who, after years of managing her type 1 diabetes, had an annual eye exam that revealed early signs of diabetic retinopathy. Due to early detection, her doctor recommended changes to her diabetes management plan, which in turn stabilized her condition—saving her from potential vision complications. To sum it up, the earlier one detects diabetic retinopathy, the better the chances of preserving vision and ensuring a good quality of life.
Common Diagnostic Tests
When it comes to diagnosing diabetic retinopathy, several screening and diagnostic tests are employed. Each test provides crucial information to healthcare providers. Here are some of the most common:
- Comprehensive Eye Examination:
- This foundational step involves dilating the pupils to allow the eye care professional to view the retina. The doctor will look for abnormal blood vessels, bleeding, and other changes in the retina.
- Fundus Photography:
- This specialized imaging technique captures detailed images of the retina, allowing for closer examinations of any swelling or abnormal structures. Pictures taken during fundus photography can also serve for future comparisons to assess disease progression.
- Optical Coherence Tomography (OCT):
- An OCT scan provides cross-sectional images of the retina, revealing its layers and allowing doctors to assess the thickness and any fluid accumulation due to macular edema. It is instrumental in understanding the severity and progression of the disease.
- Fluorescein Angiography:
- In this test, a special dye is injected into a vein in the arm, which travels to the blood vessels in the eye. Photographs are taken as the dye illuminates the blood vessels, helping doctors detect leaks, blockages, and other abnormalities.
- Visual Acuity Test:
- This basic eye test measures how well a person can see at different distances, helping gauge any impact that diabetic retinopathy might have on visual clarity.
| Diagnostic Test | Purpose |
|---|---|
| Comprehensive Eye Examination | Initial assessment of retinal health |
| Fundus Photography | Detailed images to monitor change |
| Optical Coherence Tomography (OCT) | Measures retinal thickness and fluid |
| Fluorescein Angiography | Detects blood vessel abnormalities |
| Visual Acuity Test | Assesses clarity of vision |
screenings and understanding the common diagnostic
By actively participating in regular screenings and understanding the common diagnostic tests involved, individuals with diabetes can take significant strides toward safeguarding their vision. Engaging openly with their healthcare providers about any changes in their eyesight can further enhance their proactive approach to managing diabetic retinopathy. Ultimately, convenient access to these diagnostic tests can lead to better outcomes and enhance the quality of life for those affected by diabetic retinopathy. Recognizing the importance of regular eye exams is not just a recommendation; it’s an essential step in the journey towards preserving sight and maintaining good overall health.
Read also: Simple Solutions for Headache Behind Eyes.
Treatment Options for Diabetic Retinopathy ICD 10
Having explored the significance of early detection and the various diagnostic tests for diabetic retinopathy, it’s essential to turn our focus toward treatment options. When diagnosed with diabetic retinopathy, patients often wonder about the available strategies for managing their condition. Treatment can vary significantly depending on the type and severity of the disease, but fortunately, there are several effective medical and surgical interventions.
Medical Management
Medical management is the first line of defense against diabetic retinopathy. The goal here is to control blood sugar levels, which is crucial for halting or slowing the progression of the disease. Here are the key components of medical management:
- Blood Sugar Control: This is the cornerstone of diabetic management. Keeping HbA1c levels below 7% can significantly reduce the risk of retinopathy progression. This usually involves:
- Diet and Nutrition: A balanced diet that focuses on whole grains, lean proteins, and plenty of fruits and vegetables is essential. Individuals can benefit from working with a dietitian to tailor a meal plan that supports blood sugar control.
- Physical Activity: Regular exercise helps to maintain a healthy weight and control blood sugar. Encouraging activities like walking, swimming, or cycling for 30 minutes most days can be effective.
- Medications: When lifestyle changes don’t suffice, medications might be necessary:
- Insulin Therapy: Some individuals with type 1 diabetes or advanced type 2 diabetes may require insulin to manage their blood sugar levels effectively.
- Oral Hypoglycemics: For those managing type 2 diabetes, medications like metformin or sulfonylureas may also play a role in lowering blood sugar levels.
- Regular Monitoring: Frequent check-ups with a healthcare provider can help patients track their progress. Utilizing tools like continuous glucose monitors (CGMs) can provide important feedback on blood sugar fluctuations throughout the day.
For instance, Sarah, who previously relied solely on her insulin regimen, started working with a nutritionist and implementing regular exercise into her routine. By making these lifestyle changes, she was able to improve her blood sugar levels significantly, ultimately slowing the progression of her diabetic retinopathy.
Surgical interventions for diabetic retinopathy ICD 10
In cases where diabetic retinopathy progresses to more advanced stages, surgical interventions may be necessary. These treatments aim to prevent further vision loss and address the complications caused by abnormal blood vessels. Here are some common surgical options:
- Laser Photocoagulation:
- This outpatient procedure involves using targeted laser energy to seal leaking blood vessels or shrink abnormal ones. There are two types:
- Focal Laser Treatment: Specifically targets leaking blood vessels in the retina.
- Panretinal Photocoagulation (PRP): Treats wider areas of the retina to reduce the oxygen demand of the retina and prevent new blood vessel growth.
- This outpatient procedure involves using targeted laser energy to seal leaking blood vessels or shrink abnormal ones. There are two types:
- Vitrectomy:
- This more invasive surgery is necessary when bleeding occurs in the vitreous (the gel-like substance in the eye). During vitrectomy, the surgeon removes the vitreous gel along with any blood and scar tissue that might be present.
- It helps improve vision and is typically performed when there is significant bleeding or if a retinal detachment occurs.
- Injections of Anti-VEGF Medications:
- Anti-vascular endothelial growth factor (VEGF) injections, such as ranibizumab (Lucentis) or aflibercept (Eylea), are employed to inhibit the growth of new blood vessels and can effectively treat macular edema.
Read also: Empowering Your Health Journey with an Endocrinologist’s Care
| Treatment Option | Purpose |
|---|---|
| Blood Sugar Control | Prevents and slows the progression of DR |
| Medications (Insulin/Ora) | Manages blood sugar levels |
| Laser Photocoagulation | Seals leaking blood vessels |
| Vitrectomy | Removes blood and scar tissue from the eye |
| Anti-VEGF Injections | Inhibits new blood vessel growth and treats edema |
In conclusion
a comprehensive approach combining both medical management and potential surgical interventions can empower individuals diagnosed with diabetic retinopathy to take control of their eye health. By actively engaging with healthcare providers, patients can make informed decisions, leading to improved treatment outcomes. With the right combination of lifestyle changes, medical therapies, and possibly surgical options, the risks associated with diabetic retinopathy can be effectively managed, allowing patients to preserve their vision and maintain their quality of life.
Read also: How does diabetes affect your mood?
Diagnosis and complications of diabetic retinopathy ICD 10
Having discussed the treatment options available for diabetic retinopathy, it’s important to address what lies ahead for those diagnosed with this condition. Many patients often wonder about their long-term outlook and what potential risks or complications they might face. Understanding these aspects can help individuals prepare and manage their health better.
The long-term outlook for diabetic retinopathy ICD 10
The long-term outlook for individuals with diabetic retinopathy largely depends on several factors, including the stage at which it was diagnosed, the effectiveness of treatment, and how well diabetes is managed overall.
- Early Stages: For those diagnosed with mild to moderate non-proliferative diabetic retinopathy, the prognosis is generally favorable. With diligent management of blood sugar levels, regular eye exams, and adherence to treatment plans, many can maintain good vision for years.
- Advanced Stages: The outlook becomes more concerning for individuals with proliferative diabetic retinopathy or significant macular edema. If caught early and treated appropriately with laser therapy or anti-VEGF injections, many can stabilize their condition and prevent vision loss. Regular follow-ups are crucial to monitor any progression.
- Diabetes Management: The long-term prognosis is significantly influenced by how well a person manages their diabetes. Poorly controlled blood sugar levels not only increase the risk of retinopathy progression but can also lead to a host of other complications, including kidney disease and cardiovascular issues. 4.
For example, Maria, diagnosed with diabetic retinopathy at 45, made significant lifestyle changes after her diagnosis. By prioritizing her diet, establishing a regular exercise routine, and attending all scheduled medical visits, she managed to keep her retinopathy stable for over a decade, enjoying a good quality of life and vision. The key takeaway is that proactive management of diabetes and regular monitoring of eye health play pivotal roles in determining the long-term outlook for those with diabetic retinopathy.
Potential Risks and Complications of Diabetic Retinopathy ICD 10
While there are promising strategies for maintaining eye health, it’s crucial to recognize the potential risks and complications associated with diabetic retinopathy. Some of the complications that patients may face include:
- Severe Vision Loss or Blindness: The most significant risk is the potential for vision loss. In advanced stages, diabetic retinopathy can lead to irreversible blindness, particularly if not addressed properly.
- Retinal Detachment: In severe cases of proliferative diabetic retinopathy, the fragile new blood vessels can cause scar tissue, which may lead to retinal detachment. Retinal detachment is a serious condition that requires immediate medical attention.
- Macular Edema: Swelling in the macula can occur due to leaking fluid from damaged blood vessels. If not treated, macular edema can significantly impair central vision, affecting daily activities like reading or driving.
- Recurrent Injections or Surgery: Individuals with advanced retinopathy may require repeated treatments such as anti-VEGF injections or even multiple laser surgeries, which can lead to discomfort, inconvenience, and increased healthcare costs.
| Complication | Impact |
|---|---|
| Severe Vision Loss or Blindness | Potential for irreversible blindness |
| Retinal Detachment | Requires emergency medical intervention |
| Macular Edema | Impairs central vision and daily activities |
| Recurrent Treatments | Inconvenient and may incur higher healthcare costs |
- Psychological Impact: Living with the uncertainty of diabetic retinopathy can take a toll on mental health. Anxiety over potential vision loss and awareness of needing constant eye examinations can lead to stress and emotional distress.
Frequently asked questions
What is the ICD-10 code for retinopathy of both eyes?
The ICD-10 code H35.033, which refers to bilateral hypertensive retinopathy, is a medical classification recognized by the WHO. 5.
What is the 4-2-1 rule in diabetic retinopathy?
These patients exhibit intraretinal bleeding (more than 20 in each quadrant), venous beading in two or more quadrants, or intraretinal microvascular abnormalities (IRMA) in one or more quadrants (as shown in Figure 3). This pattern is referred to as the 4:2:1 rule. It is important to note that these characteristics should be observed without any signs of neovascularization, as that would suggest proliferative diabetic retinopathy (PDR). 6.
Because your health is the most valuable thing you have and the most precious thing we care about, we always recommend that you consult your specialist doctor in everything related to your health and daily life. Everything we provide here is for awareness purposes only and does not replace consulting a doctor. Every person has a unique condition that deserves special care, and we are here by your side, working passionately to provide the information you need. Always follow us because we write for you with love and sincerity to remain a source that inspires you with hope and supports you on your journey toward a better life.
Reference



One Comment