Stroke TIA Attack: Warning Signs You Must Know
Understanding Stroke and TIA
When discussing brain health, two terms often arise: stroke and transient ischemic attack (TIA). Though they might sound similar, understanding the distinctions between the two is critical.
Differentiating between Stroke and TIA
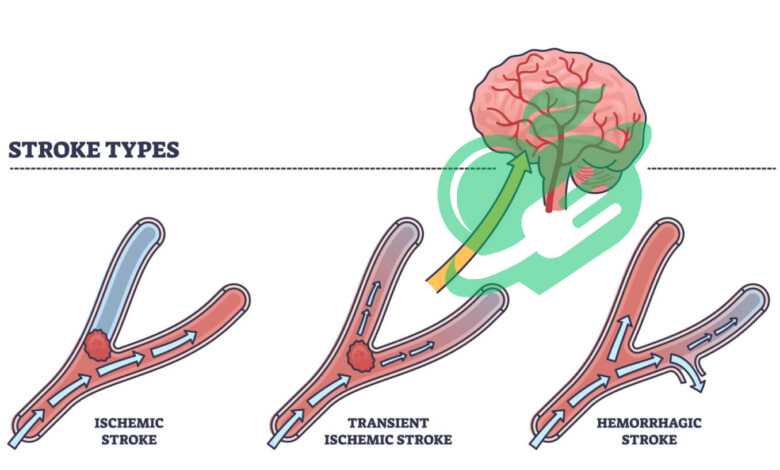
A stroke, often termed a “brain attack,” occurs when blood flow to a part of the brain is interrupted, resulting in brain cell death. This can be due to:
- Ischemic Stroke: The most common type, caused by a blood clot in a blood vessel supplying the brain.
- Hemorrhagic Stroke: Occurs when a blood vessel bursts, leading to bleeding in or around the brain.
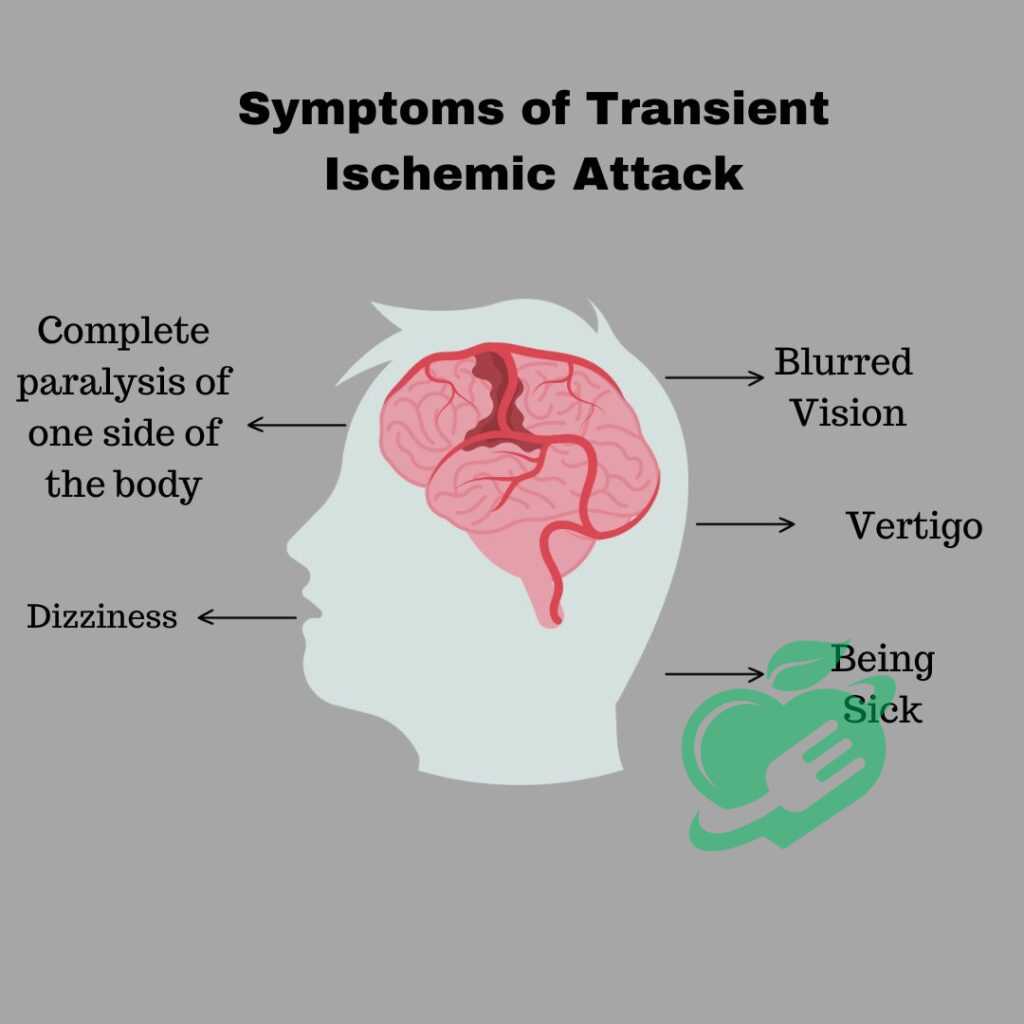
In contrast, a TIA is like a “warning sign.” Often referred to as a mini-stroke, TIAs produce similar symptoms to stroke, albeit temporarily. They typically last less than an hour, with no lasting damage to the brain. However, experiencing a TIA is a significant risk factor for a future stroke.
Causes of Stroke and TIA
Understanding the causes helps in prevention. Both stroke and TIA can stem from similar medical conditions, including:
- Atherosclerosis: Build-up of fatty deposits in arteries, narrowing blood flow.
- High Blood Pressure: Increases the risk of damage to blood vessels and the heart.
- Heart Problems: Conditions like atrial fibrillation can lead to blood clots that may travel to the brain.
Personal story: A close friend’s grandfather suffered a stroke after years of untreated high blood pressure. This moment was eye-opening, highlighting how silent conditions can lead to life-altering consequences.
Risk Factors for Stroke and TIA
Several risk factors can contribute to the likelihood of experiencing a stroke or TIA. It’s crucial to be aware and proactive about these elements. Here’s a quick rundown:
- Uncontrolled High Blood Pressure: The leading risk factor.
- High Cholesterol: Contributes to atherosclerosis, increasing the chance of clots.
- Diabetes: This condition can damage blood vessels and increase stroke risk.
- Lifestyle Choices: Smoking, a sedentary lifestyle, and excessive alcohol consumption significantly heighten risk.
- Age and Family History: Risk increases with age, and having a family history of stroke can make one more susceptible.
In summary, understanding stroke and TIA is the first step in prevention and management. Recognizing the differences, causes, and risk factors not only empowers individuals but also encourages proactive healthcare decisions. This foundational knowledge can lead to crucial lifestyle changes that may ultimately save lives.
Recognizing the Warning Signs
After understanding the mechanics of stroke and TIA, the next crucial step is recognizing their warning signs. Early detection can mean the difference between complete recovery and long-term damage or even death.
Common Symptoms of Stroke and TIA
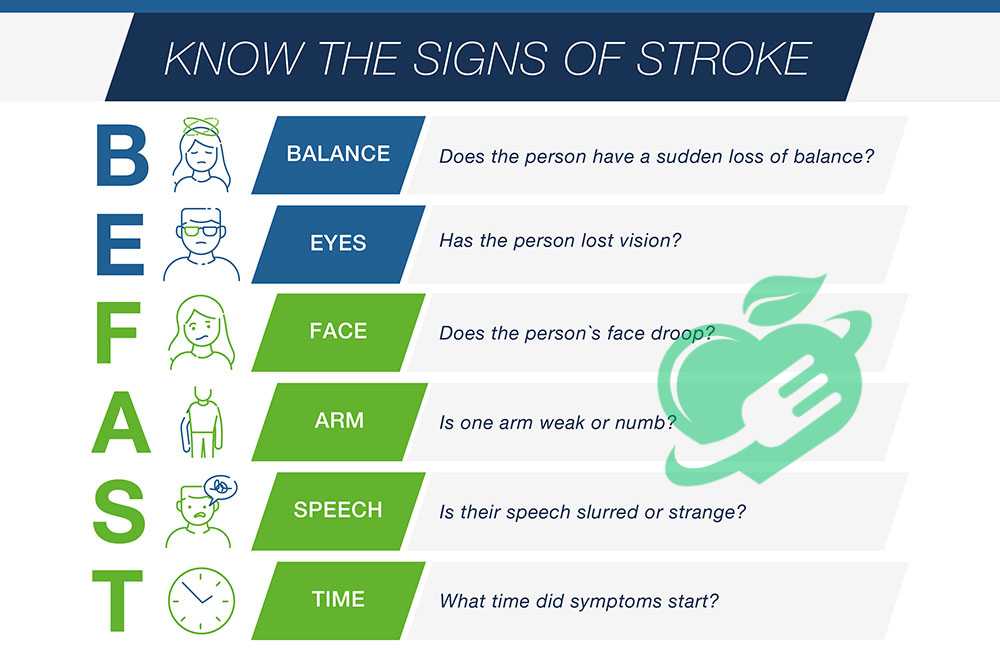
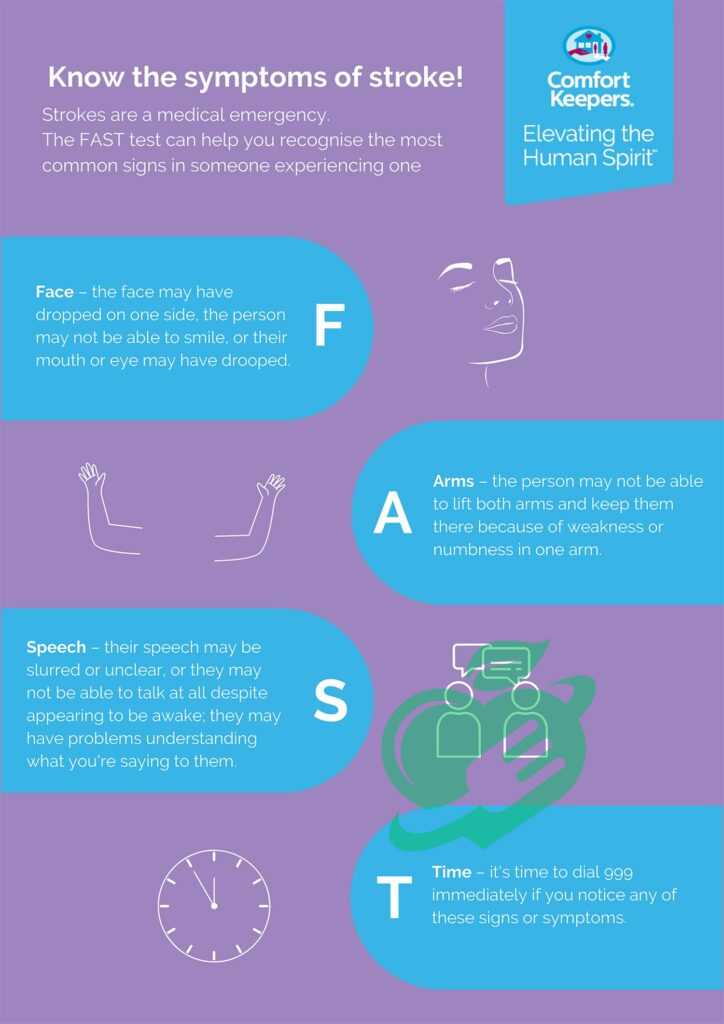
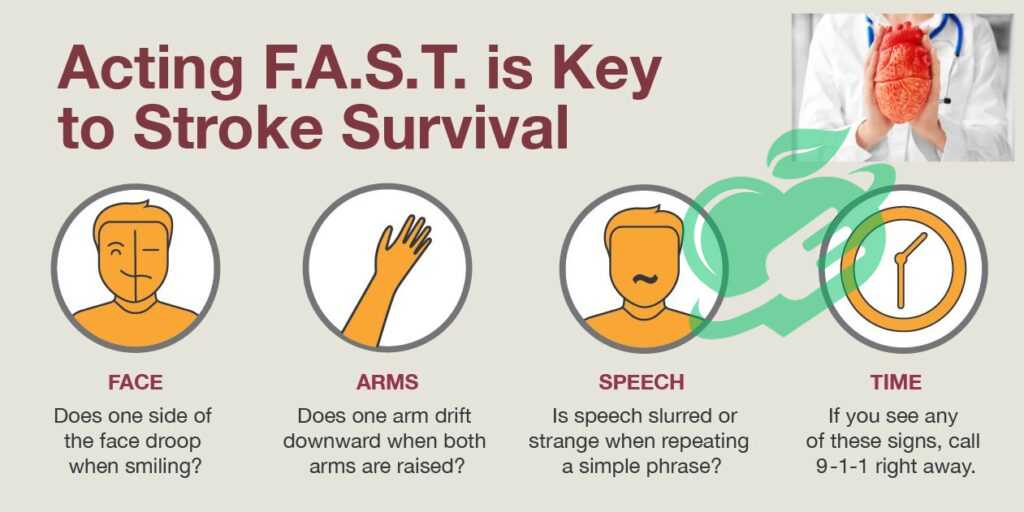
Both stroke and TIA share similar symptoms, which can appear suddenly. Being aware of these signs can empower you to act quickly. The acronym FAST is a handy guide:
- F – Face Drooping: One side of the face may droop or feel numb. Ask the person to smile. Is their smile uneven?
- A-Arm Weakness: One arm may feel weak or numb. Have them raise both arms. Does one arm drift downward?
- S – Speech Difficulty: Speech may be slurred or confused. Ask them to repeat a simple sentence. Can they do that correctly?
- T – Time to Call Emergency Services: If you notice any of these signs, it’s time to call for help immediately. 1.
Additionally, symptoms may include confusion, difficulty seeing in one or both eyes or severe headaches with no known cause. A personal experience highlights this: a friend’s colleague dismissed her sudden severe headache as a migraine, but it turned out to be a stroke.
Importance of Early Recognition
Recognizing these symptoms early is vital. Time lost is brain function lost, as every minute counts in reducing brain injury during a stroke. The sooner someone gets medical attention, the better the chance of recovery and minimizing long-term effects. Recent studies have shown that for every minute that passes without treatment during a stroke, nearly 1.9 million neurons can die. This alarming statistic emphasizes the critical nature of awareness and quick action.
When to Seek Medical Assistance
If you or a loved one begins experiencing any of the symptoms mentioned above, especially if they appear suddenly, seek medical assistance immediately. Here’s a quick checklist of situations where you should call for help:
- Sudden numbness or weakness in the face, arm, or leg, especially on one side of the body.
- Confusion or trouble understanding speech.
- Sudden trouble seeing in one or both eyes.
- A sudden severe headache with no known cause.
In summary, recognizing the warning signs of stroke and TIA plays a pivotal role in ensuring timely treatment. Understanding these symptoms and acting quickly can mean the difference between life and death or recovery and long-term disability. Empower yourself and others by spreading awareness; it could save a life.
Read also: Life After Open Heart Surgery: Tips for a Smooth Recovery
Diagnostic Procedures
Understanding the diagnostic procedures for stroke and TIA is essential for effective treatment and recovery. After recognizing the warning signs, the next step is undergoing a thorough evaluation to determine the appropriate action.
How Stroke and TIA are Diagnosed
Diagnosing stroke and TIA typically begins with a detailed medical history and physical examination. Healthcare professionals will want to know about the patient’s symptoms, duration, and any prior medical conditions. Understanding the patient’s background can help in identifying risk factors and potential causes. Common diagnostic approaches include:
- Neurological Exam: The doctor will assess the patient’s motor skills, coordination, and reflexes.
- Blood Tests: These tests can provide valuable information about blood sugar levels, cholesterol, and other critical health indicators.
It’s important to note that diagnosing TIA can be more challenging since the symptoms resolve quickly. A personal anecdote comes to mind: a family member experienced a TIA that lasted only 30 minutes. Thankfully, they sought medical attention, which led to essential follow-up tests that revealed the need for lifestyle changes to mitigate stroke risks.
Imaging Tests for Stroke and TIA
Imaging tests are crucial in confirming a diagnosis and determining the best treatment plan. Common imaging techniques include:
- CT Scan (Computed Tomography): This quick imaging test helps identify bleeding in the brain or ischemic stroke.
- MRI (Magnetic Resonance Imaging): Often considered more detailed, MRI can detect brain tissue damage that a CT scan may miss.
- Carotid Ultrasound: This test checks for blockages in the carotid arteries, which supply blood to the brain.
- Cerebral Angiography: Used in more complex cases, this test visualizes blood vessels in the brain. 2.
Each of these imaging tests provides different insights into what is happening in the brain, ultimately guiding the medical team in formulating an appropriate treatment strategy.
Read also: Brain Damage Posturing: What You Must Know
Importance of Timely Diagnosis
Timely diagnosis of stroke and TIA can drastically affect outcomes. The faster a patient receives a diagnosis and treatment, the better their chances of recovery with minimal lasting effects. Research indicates that timely intervention can significantly reduce the risk of further strokes. Every minute counts! For instance, every hour that a stroke goes untreated could lead to an increase in the permanent damage experienced. That is why understanding the diagnostic procedures and being proactive in seeking help is vital. In conclusion, being informed about how stroke and TIA are diagnosed, including necessary imaging tests, equips individuals with the knowledge to act swiftly and appropriately. Early identification can transform lives, potentially safeguarding against long-term complications and promoting a smoother path to recovery.
Read also: Preventing and Managing Brain Bleed: What You Need to Know
Treatment and Management
Once a stroke or TIA is diagnosed, the focus shifts to treatment and management. Prompt and appropriate intervention is essential to minimizing damage and facilitating recovery.
Emergency Treatment for Stroke and TIA
Emergency treatment varies depending on whether a patient is experiencing a stroke or a TIA. For strokes, particularly ischemic strokes, the most common initial treatment is thrombolysis. This involves administering a clot-busting medication called tissue plasminogen activator (tPA) within a specific time frame (usually within three to four and a half hours of symptom onset). For hemorrhagic strokes, the approach may differ. Here, the priority is controlling bleeding and reducing pressure in the brain, which might involve surgical interventions. Personal experience can solidify the importance of rapid response; a neighbor suffered a stroke and was treated quickly with tPA. Her recovery was remarkable, underscoring how critical timely emergency treatment can be.
Read also: From Panic to Recovery: Dealing with Anxiety Attack Hangover
Medications for Stroke and TIA
Following the initial emergency treatment, various medications may be prescribed depending on the type of stroke and individual patient needs. Common medications include:
- Antiplatelet Agents: Aspirin or clopidogrel can help prevent further clotting.
- Anticoagulants: For patients with certain heart conditions like atrial fibrillation, medications such as warfarin or newer anticoagulants may be recommended.
- Statins: These are often prescribed to manage cholesterol levels and reduce the risk of further strokes.
Monitoring and adjusting medications is essential, as individual responses can vary. Regular follow-ups with healthcare providers can help ensure that patients remain on the most effective regimen for their specific situation.
Rehabilitation and Lifestyle Changes
Recovery from a stroke or TIA often involves rehabilitation to regain strength and improve functionality. Rehabilitation may include:
- Physical Therapy: Aims to improve mobility and strength.
- Occupational Therapy: Focuses on daily living activities like dressing or cooking.
- Speech Therapy: Helps with communication and swallowing difficulties.
In addition to rehabilitation, lifestyle changes play a crucial role in long-term recovery and prevention of future events. Key modifications may include:
- Healthy Diet: Emphasizing fruits, vegetables, whole grains, and low-fat proteins can help manage weight and cholesterol.
- Regular Exercise: Even simple exercises can lead to significant improvements in cardiovascular health.
- Smoking Cessation: Quitting smoking dramatically lowers the risk of further strokes.
In summary, the treatment and management of stroke and TIA involve urgent interventions, appropriate medications, and ongoing rehabilitation. Each of these elements interplays to create a holistic approach to recovery, ultimately offering patients the best chance to regain their lives effectively. An awareness of the treatment pathways, combined with a commitment to lifestyle changes, can significantly enhance outcomes and overall well-being.
Read also: Choosing the Best Diet for Enhancing Brain Health

reduce the risk of stroke. It’s essential to have a thorough discussion with your healthcare provider about the best medication regimen tailored to your individual needs and risk factors.
Regular Monitoring and Follow-Up
Regular monitoring and follow-up appointments are crucial for individuals at risk of stroke or TIA. Consistent check-ups allow for early identification of potential issues and adjustments to treatment plans as necessary. Consider these key components:
- Blood Pressure Checks: Regular monitoring of blood pressure can help catch hypertension early, allowing for prompt intervention.
- Cholesterol and Blood Sugar Tests: Routine blood tests can help keep cholesterol levels and diabetes management in check, both of which are significant risk factors for stroke.
- Continuous Evaluation: Follow-ups with healthcare providers allow for ongoing assessment of medication efficacy and lifestyle modifications. This can lead to timely adjustments to prevent complications.
Personal anecdote: A friend of mine was diligent about attending her follow-up appointments after experiencing a TIA. Through these regular check-ups, her doctor was able to monitor her blood pressure and cholesterol closely. This proactive approach not only offered peace of mind but substantially reduced her risks and helped her maintain healthier habits. In conclusion, implementing effective prevention strategies can drastically reduce the likelihood of stroke and TIA. By embracing lifestyle modifications, being vigilant about medications, and prioritizing regular monitoring, individuals can take charge of their health, ensuring a brighter, healthier future. It’s never too late to start making positive changes—every small step counts in the journey toward prevention!
Read also: Brain Damage Posturing: What You Must Know
Support and Recovery
As individuals navigate the aftermath of a stroke or TIA, support and recovery play critical roles in their healing process. Understanding the resources and emotional support available can significantly improve outcomes and quality of life.
Support Systems for Stroke and TIA Patients
Having a robust support system is invaluable for anyone recovering from a stroke or TIA. Family, friends, and health professionals can provide essential assistance tailored to the needs of the individual. Here are several key support systems:
- Family and Friends: The emotional support from loved ones can be incredibly comforting. They can assist with daily tasks, encourage rehabilitation efforts, and provide companionship during recovery.
- Rehabilitation Teams: Physical, occupational, and speech therapists are critical in helping stroke survivors regain skills and independence. These professionals tailor programs to address specific challenges, helping with mobility, everyday activities, and communication skills.
- Support Groups: Connecting with others who have experienced similar challenges can foster a sense of community and understanding. Many hospitals and organizations offer support groups for stroke survivors and their families.
A personal experience highlights this: a neighbor joined a stroke support group after her husband suffered a stroke. The camaraderie and shared experiences among group members provided her with emotional comfort and practical coping strategies, making a significant difference in her journey.
Emotional and Psychological Recovery
Emotional and psychological recovery is just as important as physical recovery after a stroke or TIA. Patients may experience a myriad of emotions—anxiety, depression, frustration—due to the changes in their health status. It’s essential to address these feelings proactively:
- Counseling and Therapy: Engaging with a mental health professional can help patients work through their emotions and develop coping strategies. Cognitive-behavioral therapy (CBT) is particularly effective for addressing anxiety and depression.
- Mindfulness and Relaxation Techniques: Practices like meditation, yoga, and deep-breathing exercises can alleviate stress and improve emotional well-being.
Encouragingly, many survivors find that with time and support, their emotional health improves along with their physical recovery.
Long-Term Outlook and Prognosis
The long-term outlook for stroke and TIA patients can vary, depending on various factors like age, severity of stroke, and existing health conditions. Generally, many survivors can lead fulfilling lives with appropriate support and rehabilitation.
- Potential for Recovery: It’s essential to understand that recovery is often an ongoing process. Some individuals continue to make strides in their recovery years after the event.
- Lifestyle Changes: Adopting healthier habits can significantly enhance overall well-being and reduce the risk of future strokes or TIAs.
Frequently asked questions
What is the most common cause of TIA?
The obstruction in the blood vessels that is typically responsible for most transient ischemic attacks (TIAs) is often due to a blood clot that has formed in another part of the body and moved to the vessels that supply blood to the brain. Additionally, it can also be caused by fragments of fatty substances or air bubbles. 3.
What treatment is given for a TIA?
Platelets are cells in the blood that aid in clotting. Antiplatelet medications function by diminishing the tendency of platelets to clump together and create blood clots. Additionally, you might be prescribed other antiplatelet drugs like clopidogrel or dipyridamole. 4.
Can you stop a TIA from happening?
The most effective way to reduce the risk of a TIA is to maintain a nutritious diet, engage in regular physical activity, and avoid smoking or excessive alcohol consumption. 5.
How long does your body warn you before a stroke?
The indicators of a stroke generally appear suddenly, but they can also emerge over a period of hours or even days. This can occur when a transient ischemic attack (TIA) — a temporary blockage that resolves before causing brain damage — progresses into a stroke. 6.
Is it true that 80% of strokes can be prevented?
This is concerning as approximately 80% of strokes can be avoided. The most significant treatable risk factor for strokes is high blood pressure. It is essential to prevent, identify, and manage high blood pressure through lifestyle modifications and medication to decrease the incidence of strokes. 7.
What are the good signs after a stroke?
7 Strong Signs That Indicate You Are Making a Good Recovery from a Stroke
#1 You Achieve Your Greatest Advancement Immediately.
#2 You Are More Independent.
#3 You Can Cross Your Legs.
#4 You Notice an Increase in Your Sleep Duration.
#5 You realize there’s less necessity to rely on technique for compensation.
#6 Your Spastic Muscles Are Twitching.
7# You have experienced the process of grieving. 8.
Statistically, around one-third of stroke survivors experience ongoing challenges, but with a strong support system and proactive management, many can lead productive and meaningful lives. In summary, the journey of recovery from stroke or TIA encompasses various physical, emotional, and social. Building a comprehensive support system, prioritizing emotional health, and maintaining a positive long-term outlook can substantially aid recovery. Each step taken, no matter how small, contributes to the overarching goal of reclaiming one’s life after a stroke or TIA.
Because your health is the most valuable thing you have and the most precious thing we care about, we always recommend that you consult your specialist doctor in everything related to your health and daily life. Everything we provide here is for awareness purposes only and does not replace consulting a doctor. Every person has a unique condition that deserves special care, and we are here by your side, working passionately to provide the information you need. Always follow us, because we write for you with love and sincerity to remain a source that inspires you with hope and supports you on your journey towards a better life.



